Every year, tens of thousands of people end up in the hospital-not because their condition got worse, but because two pills they took together did something dangerous. Or because they drank grapefruit juice with their cholesterol medicine. Or because their blood thinner stopped working after they started a new antibiotic. These aren’t rare accidents. They’re drug interactions, and they’re one of the most common-and preventable-causes of medication harm.
What Exactly Is a Drug Interaction?
A drug interaction happens when something changes how a medication works in your body. That “something” could be another drug, a food, a supplement, or even an existing health condition. It doesn’t mean the medicine is broken. It means something else is interfering with how it’s absorbed, broken down, or how it acts on your body. There are three main types:- Drug-drug interactions: When two or more medications affect each other. This is the most common type-accounting for about 80% of serious cases.
- Drug-food/drink interactions: When what you eat or drink changes how a drug behaves. Grapefruit juice is the most famous example.
- Drug-condition interactions: When your health condition makes a drug riskier. For example, taking a certain blood pressure drug if you have kidney disease.
These aren’t just theoretical risks. They happen every day-and often without anyone noticing until it’s too late.
Why Drug Interactions Are So Dangerous
Imagine you’re taking warfarin (Coumadin) to prevent blood clots. It’s a delicate balance: too little, and you could have a stroke. Too much, and you could bleed internally. Now add a common antibiotic like ciprofloxacin. Suddenly, your blood thinning doubles. You don’t feel different. No warning signs. But your INR-a lab test that measures blood clotting-spikes. You end up in the ER with internal bleeding. That’s not a hypothetical. It’s happened to thousands. According to a 2022 study in JAMA Internal Medicine, serious drug interactions cause around 106,000 deaths in the U.S. each year. That’s more than car accidents or opioid overdoses. And about 6.5% of all hospital admissions are linked to medication interactions. Some drugs are especially risky. Warfarin has over 600 known interactions-including with cranberry juice, vitamin K-rich foods, and even some herbal teas. Digoxin (Lanoxin), used for heart failure, can become toxic when taken with certain antibiotics. Levothyroxine (Synthroid), taken for hypothyroidism, won’t work properly if you take it with calcium or iron supplements. Even over-the-counter meds can be dangerous. Taking ibuprofen with a diuretic can cause your kidneys to struggle. Mixing sleeping pills with alcohol? That’s a recipe for slowed breathing-or worse.How Interactions Happen: The Science Behind the Risk
Most interactions fall into two categories: pharmacokinetic and pharmacodynamic. Pharmacokinetic interactions change how your body handles the drug. Think of it like traffic on a highway. Your liver uses enzymes-especially the CYP3A4 group-to break down drugs. If one drug blocks that enzyme (like fluconazole, an antifungal), the other drug piles up. Simvastatin (Zocor), a cholesterol drug, can see its blood levels jump by 2,000% when taken with fluconazole. That’s not just a side effect-it’s a direct path to rhabdomyolysis, a life-threatening muscle breakdown. Grapefruit juice does something similar. It blocks enzymes in your gut, so more of the drug enters your bloodstream. One glass can raise statin levels by 300-600%. That’s why doctors tell you to avoid grapefruit with certain medications. It’s not a myth. It’s chemistry. Pharmacodynamic interactions are about what the drugs do together. Two sedatives? You might fall asleep and not wake up. An NSAID like naproxen with a blood pressure pill? The NSAID can make the blood pressure drug useless by causing your body to hold onto salt and water. Beta-blockers and asthma inhalers? They fight each other at the cellular level, making your asthma harder to control. Not all interactions are bad. Sometimes they’re intentional. Doctors combine drugs to boost effectiveness-like using low-dose aspirin with a statin to reduce heart attack risk. But that’s done with care, knowledge, and monitoring. Unplanned interactions? That’s where the danger lies.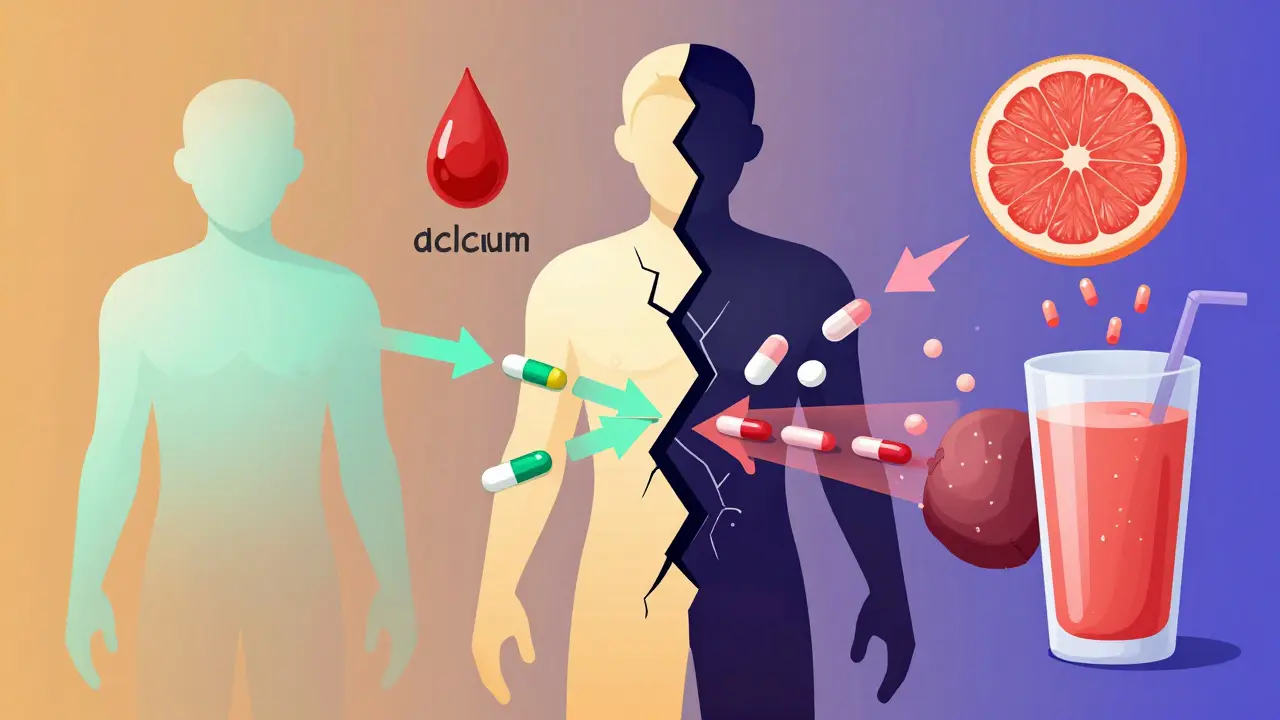
Who’s at the Highest Risk?
You might think drug interactions only affect older people. And yes, they’re more common there-but not because of age alone. People over 65 take an average of 4.7 prescription drugs daily. That’s not a typo. Four or five pills, plus supplements, plus OTC meds. The American Geriatrics Society says older adults experience drug interactions at three times the rate of younger people. The Beers Criteria-a guide for safe prescribing in seniors-lists 54 high-risk drug combinations specifically for this group. But it’s not just seniors. Anyone taking five or more medications has a 68% chance of experiencing at least one significant interaction. That includes people with diabetes, heart disease, depression, or chronic pain. And if you’re seeing multiple specialists-cardiologist, endocrinologist, neurologist-you’re at even higher risk. Each doctor sees one piece of your puzzle. Very few see the whole picture. Even young, healthy people aren’t safe. A 28-year-old taking birth control and an antibiotic for a sinus infection? That combo can reduce contraceptive effectiveness. A 30-year-old on antidepressants who starts taking St. John’s Wort? That can trigger serotonin syndrome-a rare but deadly condition.What You Can Do to Stay Safe
You don’t need a medical degree to protect yourself. Here’s what actually works:- Keep a complete list: Write down every pill, vitamin, supplement, and herb you take-including doses and when you take them. Include over-the-counter meds like ibuprofen or antacids.
- Use one pharmacy: Pharmacists are trained to spot interactions. If all your prescriptions come through one place, they can flag problems before you even walk out the door.
- Ask the pharmacist: Don’t just take the script. Ask: “Could this interact with anything else I’m taking?” They’re often the first line of defense.
- Check for food warnings: If your pill bottle says “avoid grapefruit,” don’t assume it’s just a suggestion. It’s a warning. Same with dairy products, alcohol, or high-fiber meals.
- Time your doses: If you take levothyroxine and calcium, space them at least 4 hours apart. Calcium can block absorption. Timing matters.
- Use a trusted tool: The GoodRx Drug Interaction Checker, Medscape, or the NIH’s LiverTox database are free, reliable, and updated regularly. Don’t rely on random websites or apps without medical backing.
One patient in Brisbane told me: “My pharmacist caught that my new antidepressant would clash with my blood pressure med. She called my doctor before I even took the first pill. I didn’t even know there was a risk.” That’s the kind of safety net we need more of.
The System Isn’t Perfect-And That’s the Problem
You might think electronic health records catch all this. They don’t. Only 42% of U.S. hospitals use systems that give real-time, severity-ranked alerts. The rest? They show generic warnings-or none at all. Even worse, drug companies don’t test for interactions the way they should. The FDA admits only 25% of serious interactions are found before a drug hits the market. Why? Clinical trials often exclude older adults, people with multiple conditions, or those taking other meds. So we find out the hard way-after thousands have taken it. And here’s the quiet truth: many doctors don’t know all the interactions either. A 2023 survey found less than 30% of patients get proper counseling about risks. That’s not negligence. It’s overload. Doctors see dozens of patients a day. Keeping up with 55,000+ documented interactions? Impossible.
What’s Next? The Future of Medication Safety
The good news? We’re getting better. The FDA launched the Drug Interaction Knowledgebase (DIKB) in 2023-a machine-readable database with 12,000+ verified interactions and evidence ratings. AI tools like IBM Watson are now scanning millions of patient records to find hidden patterns. And pharmacogenomics-testing your genes to see how you metabolize drugs-is becoming standard for high-risk meds like warfarin and clopidogrel. By 2026, testing for CYP450 enzyme variants will be routine for people on certain drugs. That means your medication could be tailored to your body-not just your diagnosis. But technology won’t fix everything. The real solution is better communication: between doctors, pharmacists, patients, and systems. And it starts with you asking questions.Frequently Asked Questions
Can over-the-counter medicines cause drug interactions?
Yes. Many people assume OTC meds are safe because they don’t require a prescription. But ibuprofen, naproxen, antacids, cold remedies, and even herbal supplements like St. John’s Wort or garlic pills can interfere with prescription drugs. For example, ibuprofen can reduce the effect of blood pressure medications and increase the risk of kidney damage when taken with diuretics. Always check with your pharmacist before adding any new OTC product to your routine.
Is grapefruit juice really that dangerous with medications?
For some drugs, yes. Grapefruit contains chemicals that block enzymes in your gut that normally break down certain medications. This causes much more of the drug to enter your bloodstream. With statins like simvastatin or atorvastatin, that can lead to muscle damage, kidney failure, or even death. The same applies to some blood pressure drugs, anti-anxiety meds, and immunosuppressants. If your prescription label warns against grapefruit, avoid it entirely-even small amounts matter.
Can supplements interact with my medications?
Absolutely. Supplements are not regulated like drugs, so their ingredients and potency can vary. St. John’s Wort can make birth control, antidepressants, and HIV meds less effective. Vitamin K can counteract warfarin. Calcium and iron can block thyroid medication. Even fish oil and garlic can increase bleeding risk when taken with blood thinners. Always tell your doctor and pharmacist what supplements you take-even if you think they’re "natural" or "harmless."
Why do some drug interaction checkers give different results?
Because not all databases are created equal. Professional tools like Lexicomp or Micromedex have 55,000+ interactions with detailed severity ratings and clinical evidence. Consumer apps like WebMD cover fewer interactions and often lack context. A 2022 study found that major databases only agreed on interaction severity in 63% of cases. Always use trusted, medically reviewed sources. When in doubt, ask your pharmacist.
What should I do if I think I’ve had a drug interaction?
Stop taking the medication(s) involved and contact your doctor or pharmacist immediately. If you experience symptoms like unusual bleeding, severe dizziness, chest pain, confusion, muscle pain, or trouble breathing, go to the emergency room. Don’t wait. Document everything: what you took, when, and what symptoms you noticed. Bring your complete medication list. Early intervention can prevent serious harm.
Next Steps for Safer Medication Use
If you take more than one medication, do this today:- Write down every pill, vitamin, and supplement you take-including dosages and times.
- Bring that list to your next doctor or pharmacist visit.
- Ask: “Could any of these interact with each other?”
- Use a free, reliable interaction checker like GoodRx or Medscape to double-check.
- If you’re on warfarin, digoxin, or levothyroxine, be extra careful with new meds or foods.
Medication safety isn’t just about taking your pills. It’s about understanding how they work together. One small question to your pharmacist could prevent a hospital stay. Don’t wait for a crisis to learn what you should have known.









Dayanara Villafuerte
January 18, 2026 AT 01:45Andrew Qu
January 18, 2026 AT 17:28kenneth pillet
January 20, 2026 AT 15:50Naomi Keyes
January 21, 2026 AT 13:43Andrew Short
January 21, 2026 AT 20:23Chuck Dickson
January 23, 2026 AT 06:14Robert Cassidy
January 24, 2026 AT 16:13Jodi Harding
January 26, 2026 AT 03:58Andrew McLarren
January 27, 2026 AT 04:51Emma #########
January 27, 2026 AT 05:45Kristin Dailey
January 28, 2026 AT 18:26christian Espinola
January 28, 2026 AT 19:15