One glass of grapefruit juice in the morning might seem like a healthy start to your day. But if you're taking certain medications, that habit could be putting your life at risk. This isn't a myth or an old wives' tale - it's a well-documented, potentially deadly interaction that affects more than 85 medications, with 43 of them carrying serious risks according to the U.S. Food and Drug Administration. The problem isn't the sugar or the vitamin C. It's something far more subtle: chemicals in grapefruit that silently override how your body processes drugs.
How Grapefruit Juice Changes How Your Body Handles Medications
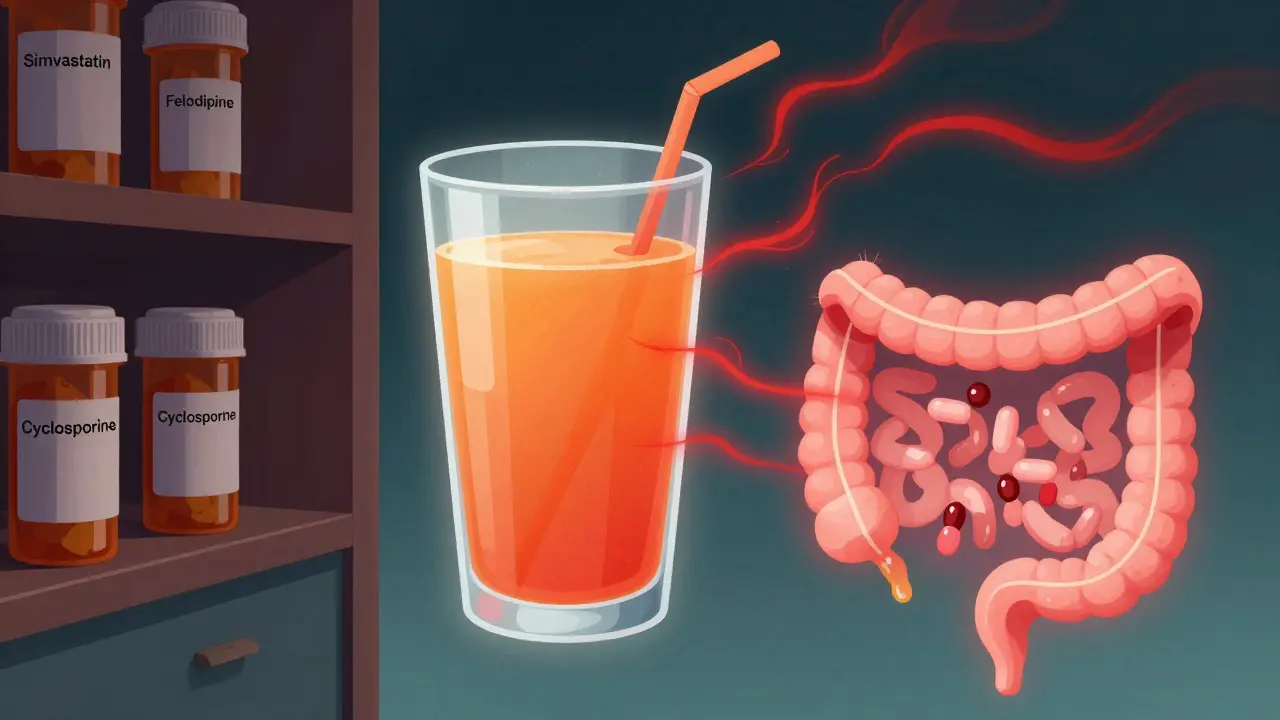
When you take a pill, your body doesn't just absorb it and send it into your bloodstream. Many drugs are broken down before they even get there - mostly by enzymes in your small intestine called CYP3A4. These enzymes act like a filter, reducing the amount of active drug that enters your system. Grapefruit juice doesn't just reduce this filter - it shuts it off.
The culprits are compounds called furanocoumarins, especially bergamottin and 6',7'-dihydroxybergamottin. These chemicals bind permanently to CYP3A4 enzymes in your gut. Once they do, those enzymes are destroyed and can't be replaced for up to 72 hours. That means if you drink grapefruit juice on Monday, your body still can't properly break down certain drugs on Wednesday. The result? Much more of the drug gets into your bloodstream than intended - sometimes up to eight times more.
This isn't a small increase. For example, a single 250mL glass of grapefruit juice can boost the blood levels of felodipine (a blood pressure drug) by 300% to 800%. With simvastatin (a cholesterol-lowering statin), the same amount increases drug exposure by 330%. That extra drug doesn't make the treatment work better - it just makes side effects more likely and more dangerous.
Which Medications Are Most at Risk?
Not all drugs are affected the same way. The risk depends on whether the drug is heavily processed by CYP3A4 in the gut. Here are the main categories where grapefruit juice can cause real harm:
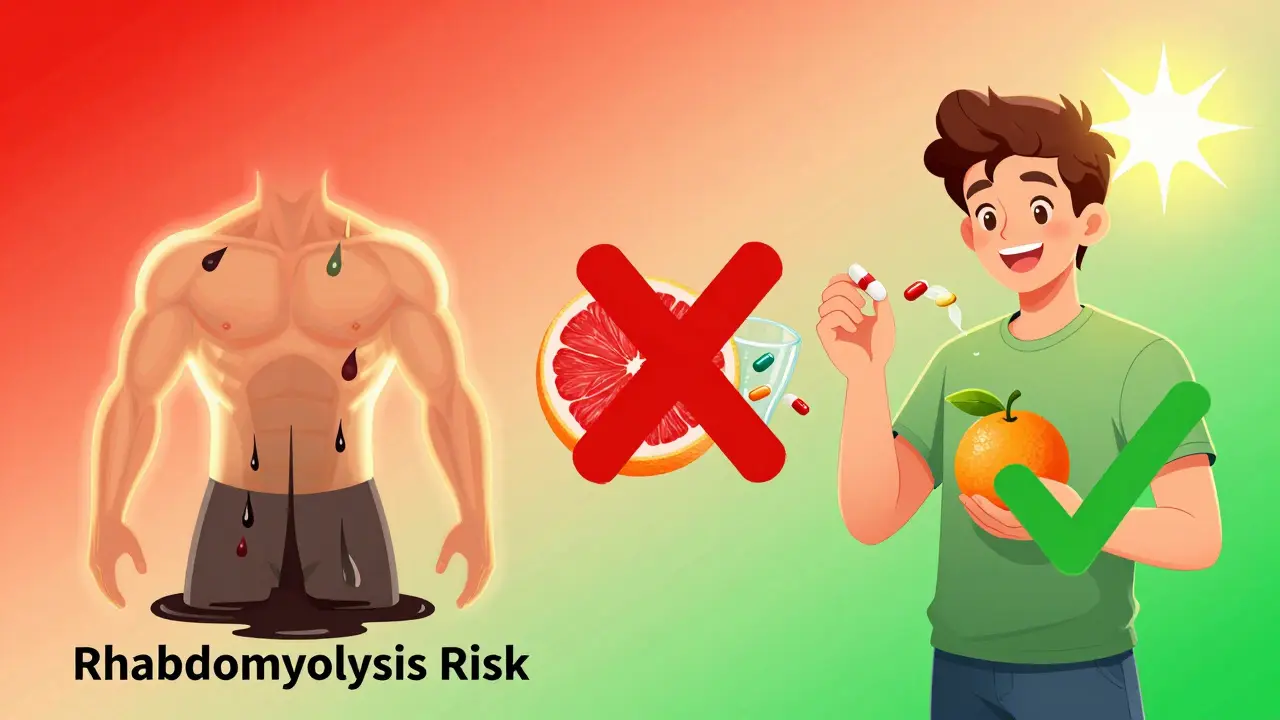
- Statins: Simvastatin and lovastatin are high-risk. A single glass can cause muscle breakdown (rhabdomyolysis), which can lead to kidney failure. Atorvastatin has a moderate risk. But pravastatin, rosuvastatin, and fluvastatin? No interaction. They use different metabolic pathways.
- Calcium channel blockers: Felodipine, nifedipine, and verapamil can cause dangerously low blood pressure or irregular heart rhythms. Amlodipine, however, is safe - it doesn't rely on CYP3A4.
- Benzodiazepines: Oral midazolam and triazolam can cause extreme drowsiness, confusion, or even respiratory depression when mixed with grapefruit.
- Immunosuppressants: Cyclosporine and tacrolimus - used after organ transplants - can reach toxic levels, damaging kidneys or the nervous system.
- Antiarrhythmics: Amiodarone can lead to fatal heart rhythm disturbances.
- Some antidepressants and antipsychotics: Sertraline, quetiapine, and buspirone can cause serotonin syndrome or excessive sedation.
Some drugs even behave oddly - like theophylline or itraconazole - where grapefruit juice actually lowers their levels, making them less effective. But these cases are rare. The overwhelming majority of interactions are dangerous increases in drug levels.

Not All Citrus Is the Same
If you're told to avoid grapefruit, you might wonder: What about oranges? Or tangerines? The good news is, regular sweet oranges and tangerines don't contain furanocoumarins. They're safe. Even blood oranges and navel oranges pose no risk.
But Seville oranges - the kind used in traditional marmalade - are just as dangerous as grapefruit. So are pomelos, which are large, pithy citrus fruits closely related to grapefruit. Even if you think you're being careful, consuming marmalade made from Seville oranges while taking simvastatin or cyclosporine is just as risky as drinking grapefruit juice.
And it doesn't matter how you take it. Fresh fruit, frozen concentrate, or freshly squeezed juice - they all contain the same harmful compounds. Even a small amount, as little as 200mL (about 6.8 fluid ounces), is enough to trigger an interaction. There's no "safe" amount if you're on a high-risk medication.
Why This Interaction Is So Hard to Avoid
One of the biggest problems is that most people don't know they're at risk. A 2021 study found that only 28% of patients could correctly name which of their medications interacted with grapefruit - even though 65% had been told to avoid it. Many assume it's just a "warning on the label" and don't think it applies to them.
Doctors often don't bring it up. Pharmacists, despite being the most likely to know, only consistently warn patients about 37% of the time, according to research published in Clinical Pharmacology & Therapeutics. And even when warned, 47% of patients continue to consume grapefruit products. For people over 65, that number jumps to 63%.
Why? Because the effects aren't immediate. You don't feel sick right after drinking the juice. The danger builds slowly - over hours or days. A patient might take their statin with grapefruit juice for weeks before suddenly experiencing muscle pain or dark urine - signs of rhabdomyolysis. By then, it's too late.
What You Should Do If You're on Medication
If you're taking any prescription drug, especially for high blood pressure, cholesterol, heart rhythm, or after an organ transplant, here’s what to do:
- Check your medication label. Look for warnings about grapefruit juice. As of 2021, about 19% of prescription labels in the U.S. include this warning - up from 12% in 2015.
- Ask your pharmacist. Don't assume. Bring your full list of medications to the pharmacy and ask: "Which of these can't I take with grapefruit?"
- Assume it's risky unless proven otherwise. If you're unsure, avoid grapefruit entirely. It's safer than guessing.
- Wait 72 hours. If you accidentally drink grapefruit juice, don't take your medication for at least three days. The enzyme damage lasts that long.
- Switch to a safer alternative. Many drugs have versions that don't interact. For example, switch from simvastatin to rosuvastatin or pravastatin. Your doctor can help.
There are also new tools helping patients. Electronic health records now include over 128 grapefruit interaction alerts. Drug interaction apps and pharmacy systems flag these risks automatically. But they're only as good as the data entered. You still need to be your own advocate.
The Bigger Picture: Why This Matters Now
This isn't just about one fruit. It's about how easily we overlook hidden risks in our daily routines. Older adults - who are more likely to take multiple medications - are especially vulnerable. In the U.S., 42% of adults over 40 take at least one drug affected by grapefruit juice. In Australia, where I live, the same pattern holds true.
The European Medicines Agency estimates grapefruit interactions cause about 85 serious adverse events each year in Europe, with 12 deaths between 2000 and 2019. The American Geriatrics Society includes grapefruit interactions in their 2023 Beers Criteria - a list of potentially dangerous medications for older adults.
Even the pharmaceutical industry is responding. Some drugmakers have reformulated medications - like extended-release felodipine - to reduce the interaction. Others are testing CRISPR gene editing to create furanocoumarin-free grapefruit varieties. But none of that helps if you're still drinking the juice.
The bottom line is simple: if your medication has even a small chance of interacting with grapefruit, don't take the risk. The consequences aren't theoretical. They're documented. They're deadly. And they're entirely preventable.
Can I drink grapefruit juice if I take my medication at night?
No. The enzyme inhibition from grapefruit juice lasts up to 72 hours. Taking your medication at night doesn't help if you drank grapefruit juice in the morning - or even two days ago. The damage to your intestinal enzymes is permanent until your body makes new ones, which takes about three days.
Is grapefruit juice the only citrus fruit that causes problems?
No. Seville oranges (used in marmalade) and pomelos contain the same harmful compounds. Regular oranges, tangerines, and clementines are safe. Blood oranges are also fine. Always check the type - not just the color.
What if I only drink a small amount of grapefruit juice?
Even 200mL - about one small glass - is enough to cause a dangerous interaction. There's no safe threshold. The effect is not dose-dependent in the way you might expect. One glass can shut down your enzyme system for days.
Can I take grapefruit juice and my medication hours apart?
For CYP3A4 interactions (the most common), no. The enzyme damage lasts three days. For OATP-mediated interactions (like with fexofenadine), a 4-hour gap may help - but those are rare. If you're unsure, avoid grapefruit entirely.
Are there safe alternatives to grapefruit juice?
Yes. Orange juice, apple juice, cranberry juice, and water are all safe. If you're taking a statin, switching from simvastatin to rosuvastatin or pravastatin removes the risk entirely. Talk to your doctor about alternatives - many exist.









Teresa Marzo Lostalé
December 28, 2025 AT 13:30Ellen-Cathryn Nash
December 29, 2025 AT 09:18Samantha Hobbs
December 29, 2025 AT 16:00Nicole Beasley
December 30, 2025 AT 21:39sonam gupta
January 1, 2026 AT 02:05Julius Hader
January 1, 2026 AT 11:23James Hilton
January 2, 2026 AT 19:58Mimi Bos
January 3, 2026 AT 01:56Kelsey Youmans
January 3, 2026 AT 12:51Sydney Lee
January 5, 2026 AT 05:44oluwarotimi w alaka
January 6, 2026 AT 17:24Debra Cagwin
January 8, 2026 AT 13:51Hakim Bachiri
January 9, 2026 AT 22:51Celia McTighe
January 11, 2026 AT 01:14Ryan Touhill
January 12, 2026 AT 01:29