Every year, thousands of people end up in the hospital not because their medication didn’t work, but because something they ate, drank, or took as a supplement changed how that medicine acted in their body. It’s not rare. It’s not exotic. It’s happening right now to someone you know-maybe even you. A glass of grapefruit juice with your statin. A daily garlic pill while on blood thinners. St. John’s wort for low mood while taking antidepressants. These aren’t just "maybe" risks. They’re proven dangers with real consequences: muscle breakdown, uncontrolled bleeding, heart rhythm problems, or even treatment failure for serious conditions like HIV or organ transplant rejection.
What Exactly Is a Drug Interaction?
A drug interaction happens when something-food, drink, another pill, or a supplement-changes how your medication works. It doesn’t mean the medicine is broken. It means something else is interfering with it. There are three main types:- Drug-drug interactions: One prescription or over-the-counter medicine affects another.
- Drug-food interactions: What you eat or drink changes how your body absorbs or breaks down the drug.
- Drug-supplement interactions: Vitamins, herbs, minerals, or herbal products alter your medication’s effect.
These aren’t theoretical. The FDA says about 40% of American adults take dietary supplements. In Australia, that number is close. And with most people taking at least one prescription med, the chances of a clash are high. About 3-5% of all hospital admissions are linked to preventable drug interactions. That’s tens of thousands of people every year-many of them older adults managing multiple conditions.
How Do Interactions Actually Happen?
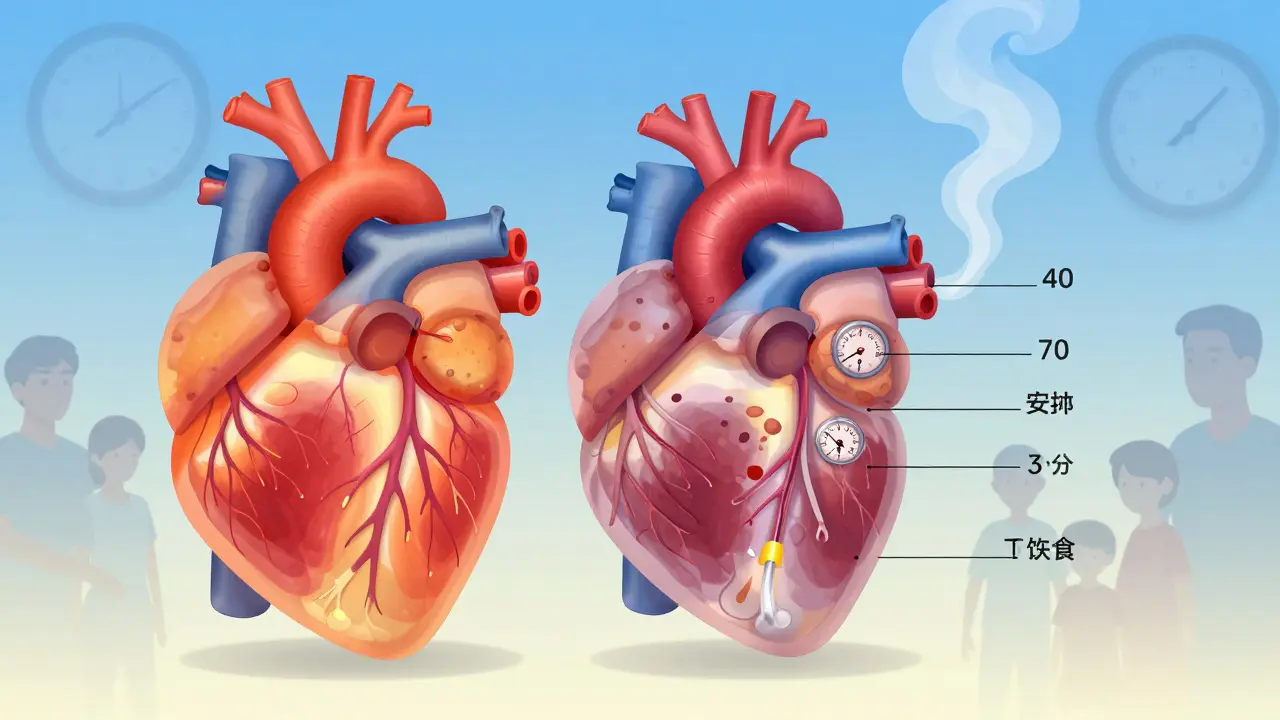
Your body doesn’t treat pills like magic bullets. It breaks them down, moves them around, and gets rid of them using a complex system. Most interactions happen in one of two ways: through your liver’s enzymes or by changing how your body responds to the drug.Pharmacokinetic interactions affect how your body handles the drug. The most common culprit? The cytochrome P450 enzyme system-especially the CYP3A4 enzyme. This enzyme breaks down about half of all prescription drugs. If something blocks it, the drug builds up in your blood and can become toxic. If something speeds it up, the drug gets cleared too fast and stops working.
St. John’s wort is the poster child for this. It’s a popular herb for mild depression, but it’s also a powerful activator of CYP3A4. Take it with cyclosporine (used after transplants), and your body flushes out 50-70% of the drug in just two weeks. That means your body might reject the new organ. Take it with birth control pills, and your risk of unintended pregnancy jumps by 50-70%. Take it with SSRIs like sertraline or fluoxetine, and you could trigger serotonin syndrome-a medical emergency with high fever, shaking, confusion, and muscle stiffness.
Pharmacodynamic interactions are about what the drug does to your body. If two things do the same thing, they can overdo it. If they do opposite things, they cancel each other out.
For example, hawthorn (used for heart health) and digoxin (used for heart failure) both strengthen heart contractions. Together, they can overwork the heart. Or take warfarin (a blood thinner) with ginkgo biloba or garlic supplements-both thin the blood too. Add them together, and you’re playing Russian roulette with internal bleeding. There are over 30 documented cases of major bleeding in people who combined warfarin with garlic supplements.
The Silent Killer: Grapefruit Juice
Grapefruit juice is the most dangerous food you might be drinking with your meds-and most people have no idea. It’s not about sugar. It’s about furanocoumarins, chemicals that permanently shut down CYP3A4 enzymes in your gut. That means your body can’t break down the drug before it enters your bloodstream.With simvastatin (a cholesterol drug), one glass of grapefruit juice can raise blood levels by up to 15 times. That turns a safe dose into a toxic one. The risk of rhabdomyolysis-a condition where muscle tissue breaks down and floods your kidneys with dangerous proteins-goes from 0.15 cases per 100,000 people per year to 1.57. That’s a tenfold increase.
It’s not just grapefruit. Seville oranges, pomelos, and some tangelos do the same thing. And it doesn’t matter if you drink it hours before or after your pill. Once the enzyme is blocked, it stays blocked for 24-72 hours. No amount of timing fixes it.
Statins aren’t the only ones affected. Blood pressure meds like felodipine, anti-anxiety drugs like buspirone, and even some cancer drugs can become dangerously concentrated if you drink grapefruit juice.

Warfarin and Vitamin K: The Balancing Act
Warfarin is one of the most common blood thinners. It works by blocking vitamin K, which your body needs to make clotting factors. So if you suddenly eat a lot of vitamin K, warfarin can’t do its job.Leafy greens-spinach, kale, broccoli, Brussels sprouts-are packed with vitamin K. One cup of cooked spinach has about 830 micrograms. That’s more than 8 times the daily recommended intake. If you suddenly start eating that every day, your INR (a blood test that measures clotting time) can drop by 30-40% in 24 hours. That means your blood clots faster. You’re at risk for stroke or a blood clot in your lungs.
The fix? Don’t stop eating greens. Just keep your intake consistent. If you normally eat a salad a few times a week, keep doing that. If you never eat them, don’t suddenly start. The goal isn’t to avoid vitamin K-it’s to keep your levels steady. The National Academy of Medicine recommends 90mcg per day for women and 120mcg for men. That’s about one cup of cooked kale or two cups of raw spinach. You don’t need to count it. Just avoid wild swings.
And don’t assume cranberry juice is safe. Between 2003 and 2015, there were at least 28 published cases of people on warfarin who had dangerous bleeding after drinking cranberry juice. Their INR spiked above 8.0-normal is 2.0-3.0. That’s life-threatening.
Supplements That Can Hurt You
Supplements aren’t regulated like drugs. That means no proof of safety, no required warnings, and no guarantee they contain what’s on the label. But some are known to be dangerous with common meds.- St. John’s wort: Interacts with over 50% of prescription drugs. Reduces effectiveness of HIV meds, birth control, antidepressants, and transplant drugs.
- Ginkgo biloba: Increases bleeding risk with warfarin, aspirin, and clopidogrel. Can cause brain bleeds.
- Garlic supplements: 32 documented cases of bleeding when taken with blood thinners. Even raw garlic in large amounts can do this.
- Red yeast rice: Contains natural statins. If you’re already on a statin like atorvastatin, taking this can cause severe muscle damage.
- Coenzyme Q10: May reduce statin effectiveness. Some people take it to fight statin side effects-but it might make the drug less protective.
- Green tea: High in vitamin K. Can interfere with warfarin. Also contains caffeine, which can raise blood pressure and interfere with some heart meds.
The problem? Most people don’t think of supplements as medicine. They say, “It’s natural, so it’s safe.” But natural doesn’t mean harmless. The FDA reports that between 2004 and 2013, adverse event reports involving supplements jumped 45%. Nearly a quarter of those were due to interactions.

What You Can Do: A Simple Action Plan
You don’t need to be a pharmacist to protect yourself. Here’s what works:- Make a full list: Write down every pill, vitamin, herb, and supplement you take-even if you only take it once a week. Include over-the-counter stuff like ibuprofen or antacids.
- Bring it to every appointment: Doctors don’t ask about supplements unless you tell them. Studies show 70% of patients don’t mention them. Don’t assume they know. Show the list. Take a photo of the bottles if you need to.
- Ask your pharmacist: Pharmacists are trained to catch interactions. They see your full medication history. Ask: “Is this safe with everything else I take?”
- Use free tools: The FDA’s MedlinePlus drug interaction checker lets you enter up to 10 medications and supplements. It flags risks in plain language. No sign-up needed.
- Don’t start new supplements without asking: Even “safe” ones like fish oil or magnesium can interact. If you’re on a blood thinner, fish oil can increase bleeding risk. Magnesium can lower blood pressure too much if you’re already on meds for it.
Why This Matters More Than You Think
This isn’t just about avoiding side effects. It’s about keeping your treatment effective. If your blood thinner stops working because of a supplement, you could have a stroke. If your transplant drug drops too low, your body could reject the organ. If your antidepressant stops working because of St. John’s wort, you could spiral into depression.And the cost? The Institute for Safe Medication Practices estimates drug-supplement interactions cost the U.S. healthcare system $177 billion a year in preventable hospital visits, ER trips, and lost work. That’s not just money. It’s lives.
There’s good news. Hospitals using clinical decision support tools like Epic’s interaction checker reduced dangerous prescribing by 37%. Pharmacists doing full medication reviews cut adverse events by 22%. Patients who got clear education about warfarin and diet kept their INR in range 68% of the time-compared to 42% for those who didn’t.
You don’t need to be an expert. You just need to be informed. And you need to speak up.
Final Thought: Your Medicine Isn’t Just the Pill
Your body doesn’t care if something is called a drug, a vitamin, or a tea. It only cares about the chemicals inside. A supplement bottle doesn’t come with a warning label like a prescription does. That’s why the responsibility falls on you.Don’t assume. Don’t guess. Don’t rely on Google searches or advice from friends. Ask your doctor. Ask your pharmacist. Show them your list. Keep it updated. That simple habit could save your life-or prevent you from needing a hospital bed entirely.
Can I still drink grapefruit juice if I take medication?
If you take certain medications-like statins (simvastatin, atorvastatin), some blood pressure drugs (felodipine), anti-anxiety meds (buspirone), or certain cancer treatments-you should avoid grapefruit juice entirely. Even one glass can cause dangerous buildup of the drug in your blood. The effect lasts up to 72 hours. If you’re unsure, check with your pharmacist or use the MedlinePlus interaction checker. For most other medications, it’s safe, but it’s always better to ask.
Are herbal supplements safer than prescription drugs?
No. Just because something is natural doesn’t mean it’s safe. Herbs like St. John’s wort, ginkgo, and garlic can be just as powerful-and just as dangerous-as prescription drugs. They’re not tested for safety the same way, and they’re not required to list side effects or interactions. In fact, St. John’s wort is so potent it can make birth control fail or cause transplant rejection. Treat supplements like medicine: ask before you take them.
Should I stop eating spinach if I’m on warfarin?
No. You don’t need to stop eating spinach or other leafy greens. What matters is consistency. If you normally eat a salad twice a week, keep doing that. If you never eat them, don’t suddenly start eating large amounts every day. Sudden changes in vitamin K intake can make warfarin less effective. The goal is stable intake-not avoidance. Aim for about 90-120mcg of vitamin K per day, which is roughly one to two cups of raw spinach or half a cup of cooked kale.
Can I use a drug interaction checker app?
Yes, and you should. The free MedlinePlus drug interaction checker from the U.S. National Library of Medicine lets you enter up to 10 medications and supplements. It tells you in plain language whether there’s a risk and how serious it is. Other apps exist, but stick to ones backed by government or medical institutions. Don’t rely on commercial apps that push products or ads.
Why don’t supplement labels have interaction warnings?
Because they’re not required to. Under current U.S. law (DSHEA, 1994), supplements are classified as food, not drugs. That means they don’t need FDA approval before sale, and they don’t need to list side effects or interactions. Only 29% of supplement labels include any warning about drug interactions. That’s why it’s up to you to ask your pharmacist or doctor before taking anything new.
What if I forgot to tell my doctor about a supplement I’m taking?
It’s never too late to speak up. Call your doctor’s office or pharmacist and say, “I forgot to mention I’ve been taking [name of supplement]. Is that safe with my other meds?” Most clinics have a nurse or pharmacist on staff who can check it for you within a day. Don’t wait until you feel sick. Even if you’ve been taking it for months, telling them now can prevent a problem before it starts.






lisa Bajram
January 11, 2026 AT 16:31Okay but let’s be real-grapefruit juice is the silent villain of every elderly person’s medicine cabinet. My grandma took her statin with it for YEARS until her pharmacist nearly had a heart attack. She thought it was ‘healthy.’ Now she drinks orange juice and calls it a day. Simple fix, huge difference.
Jaqueline santos bau
January 13, 2026 AT 02:47OMG I JUST REALIZED I’VE BEEN TAKING ST. JOHN’S WORT WITH MY ANTIDEPRESSANTS FOR 8 MONTHS. IS IT TOO LATE? I FEEL FINE BUT WHAT IF I’M ONE HEARTBEAT AWAY FROM SEROTONIN SYNDROME?? SOMEONE TELL ME I’M NOT GOING TO DIE.
Aurora Memo
January 15, 2026 AT 02:35I appreciate how clear this post is. I used to think supplements were harmless because they’re ‘natural.’ Now I bring my pill bottles to every appointment-even the gummy vitamins. My pharmacist caught a conflict between my blood pressure med and my magnesium supplement. Saved me from a fall.
Faith Edwards
January 16, 2026 AT 15:11It is profoundly disconcerting to observe the pervasive cultural disregard for pharmacological integrity in the context of over-the-counter dietary adjuncts. The notion that ‘natural’ equates to ‘benign’ is not merely erroneous-it is a perilous epistemological fallacy, one which has precipitated a veritable public health crisis of iatrogenic origin. One must, therefore, exercise the utmost diligence in the procurement and administration of such substances, lest one become an unwitting participant in a biochemical catastrophe.
Jay Amparo
January 17, 2026 AT 13:51My mom in India takes turmeric for arthritis and warfarin for AFib. She didn’t know they could clash. I showed her this post and now she tells her doctor before taking anything-even ‘just a pinch’ of spice. We need more of this info in languages other than English. This could save lives in villages where people think ‘no label = no risk.’
Lisa Cozad
January 18, 2026 AT 14:33Just started taking CoQ10 because my doc said it helps with statin muscle pain. Then I read this and panicked. Called my pharmacist-turns out it’s fine at low doses, but I should avoid high-dose stuff. So glad I asked. Don’t assume. Just ask.
Saumya Roy Chaudhuri
January 20, 2026 AT 04:17Everyone’s freaking out about grapefruit juice but nobody talks about green tea. It’s got vitamin K AND caffeine AND catechins that mess with liver enzymes. I’ve seen three patients with INR spikes from ‘healthy’ green tea extract capsules. You think you’re being good, but you’re just another walking interaction waiting to happen.
Ian Cheung
January 21, 2026 AT 05:57My uncle took garlic pills with his blood thinner and ended up in the ER with a brain bleed. He swore he was ‘just trying to be healthy.’ Now he’s on a feeding tube. Don’t be him. Don’t be me. Don’t be anyone who thinks ‘natural’ means ‘safe.’ Just ask. Always ask.
anthony martinez
January 21, 2026 AT 06:48So let me get this straight. I can’t drink grapefruit juice, take garlic, eat spinach, or breathe near St. John’s wort without risking death or transplant rejection? Cool. So what’s left? Water? And maybe aspirin if I’m feeling spicy. Thanks for the checklist, doc. I’ll just stop taking everything and hope for the best.
Ashlee Montgomery
January 23, 2026 AT 02:56It’s interesting how we treat drugs like sacred objects and supplements like harmless snacks. But the body doesn’t distinguish between ‘prescription’ and ‘herbal’-it only sees chemistry. Maybe the real issue isn’t the interactions, but our cultural refusal to treat all bioactive substances with equal respect.
Ritwik Bose
January 24, 2026 AT 17:42Thank you for this detailed and thoughtful exposition. I have shared this with my elderly parents in the U.S. and my relatives in India. Many do not realize that supplements are not regulated. I have encouraged them to carry a printed list of all medications and supplements to every medical visit. A small step, but potentially life-saving.
Paul Bear
January 24, 2026 AT 19:07Correction: The FDA does not say ‘about 40% of American adults take dietary supplements.’ The NHANES 2017–2020 data shows 76.7% of U.S. adults report using at least one dietary supplement. Also, the 3–5% hospital admission statistic is from the Journal of the American Pharmacists Association, not the FDA. Accuracy matters. This post is otherwise excellent.