When you or a loved one can’t understand what the doctor or pharmacist is saying about your medicine, it’s not just frustrating-it’s dangerous. Every year, thousands of people in the U.S. end up in the hospital or worse because they misunderstood their medication instructions. This isn’t about bad luck. It’s about language barriers-and how the system keeps failing people who don’t speak English fluently.
Why Language Barriers Lead to Medication Errors
Imagine getting a prescription for insulin. The label says "take one unit at bedtime." But you don’t know what "unit" means. Or worse, the pharmacist gives you instructions in English, and you nod along because you don’t want to seem confused. Later, you take five units because you thought "one unit" meant one drop. That’s not hypothetical. That’s what happened to a Spanish-speaking woman in Texas in 2022. Her family used Google Translate to read the label. She ended up in the ER with dangerously low blood sugar. Studies show that patients with limited English proficiency (LEP) are twice as likely to have a medication error compared to English-speaking patients. For children in LEP households, the risk jumps even higher-17.7% experience an adverse event versus 9.6% for others. These aren’t just numbers. They’re kids who missed doses, adults who took double the amount, or elderly patients who didn’t know when to refill. The problem isn’t just translation. It’s context. Words like "dropperful," "take with food," or "for thirty days" don’t always translate clearly-even with apps. Pharmacies in places like the Bronx and Milwaukee still can’t print prescription labels in Spanish, even though most of their patients speak it. And when staff don’t know how to identify LEP patients before they arrive, the system breaks before it even starts.What Actually Works: The Best Ways to Get Help
You don’t have to guess or rely on family members who don’t know medical terms. There are proven, safe ways to get help. Professional interpreters-in person, over the phone, or by video-are the gold standard. Research shows they cut medication errors by up to 50%. That’s not a small improvement. It’s life-saving. A hospital in Philadelphia cut its LEP medication errors by 40% in just one year after hiring certified medical interpreters for every appointment. Avoid using family members, friends, or children as interpreters. One in nine pharmacies still rely on them, and studies show that nearly a quarter of those interpretations are wrong. Kids shouldn’t be translating insulin doses. Spouses shouldn’t be guessing dosage schedules. This isn’t cultural-it’s clinical. Directly observed dosing is another powerful tool. If you’re taking a high-risk medication like blood thinners or chemotherapy, ask the nurse or pharmacist to watch you take your first dose. Have you say back what you’re supposed to do. This simple step catches misunderstandings before they cause harm. Translated materials matter too. Prescription labels, warning sheets, and refill instructions should be available in the top languages spoken in your area. If your pharmacy doesn’t offer them, ask for them. If they say no, ask to speak to the manager. Under federal law, they’re required to provide language help.What You Can Do Right Now
You don’t need to wait for the system to fix itself. Here’s what you can do today:- Always say you need an interpreter when you arrive. Don’t wait to be asked. Say: "I need a professional interpreter for my appointment."
- Ask for written instructions in your language. If they don’t have them, ask if they can email or text them to you.
- Use the teach-back method: After the provider explains your medicine, say, "Can you please explain it back to me so I make sure I understand?" Then say it in your own words.
- If you’re using a phone or video app for your appointment, check if the platform has a built-in interpreter option. Most hospital portals now do.
- Keep a list of your medications, dosages, and times in your language. Show it to your provider every visit.

What Hospitals and Pharmacies Should Be Doing
It’s not enough to say they "offer" interpretation. They need to make it automatic. The best systems do three things:- Ask every patient at check-in: "What language do you prefer to speak?" This is required by The Joint Commission.
- Have trained interpreters available within five minutes, whether in person or via video.
- Translate all high-risk medication instructions-insulin, blood thinners, seizure meds-into the top five languages spoken in their community.
Legal Rights and What to Do If You’re Denied Help
You have a legal right to language assistance. Title VI of the Civil Rights Act says any healthcare provider receiving federal funds-meaning almost every hospital and pharmacy-must provide free interpreter services. You don’t pay for it. You don’t ask for permission. You ask for it. If you’re told, "We don’t have an interpreter," say: "I know this is required by law. Can you please connect me to your language services department?" If they still refuse, ask for the patient advocate or file a complaint with the Office for Civil Rights. You can do this anonymously. Some states, like California and New York, have stronger laws. If you’re in one of those states, you can also call your state’s health department hotline. They’ll help you get what you’re legally owed.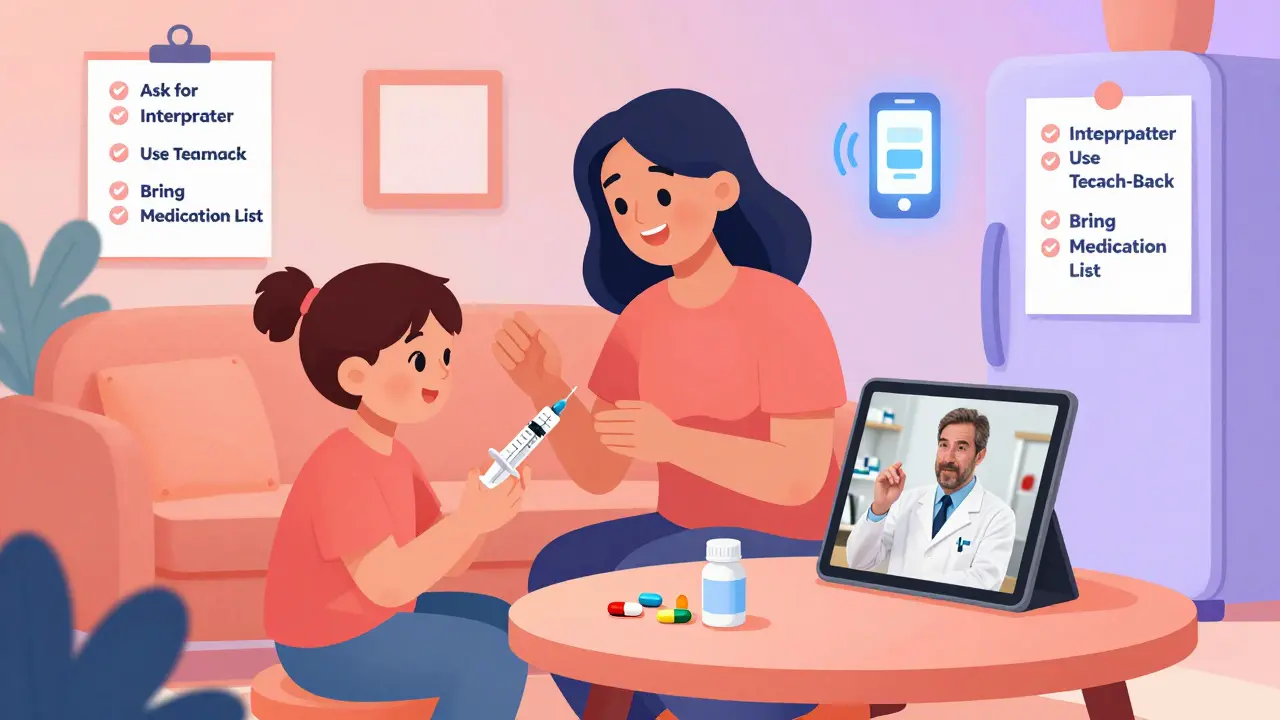
What’s Changing for the Better
The tide is turning. In 2022, Medicare started paying for remote interpreter services during telehealth visits. In 2023, the FDA announced it will require multilingual labeling on high-risk medications by 2024. Epic and Cerner, the two biggest electronic health record systems, are rolling out new tools in 2024 that automatically flag LEP patients and connect them to interpreters. AI-powered translation tools for medication instructions are being tested by the NIH. They’re not perfect yet-but they’re getting better. For now, human interpreters are still the safest option.Real Stories: What Happens When Help Is Given-and When It’s Not
One woman in Chicago had her husband’s diabetes medication misread because the pharmacy used a teenager to interpret. He ended up in the hospital with nerve damage. After that, she started bringing a printed list of his meds in Spanish to every visit. She also asked for a video interpreter. Within three months, her husband’s blood sugar stabilized. Another family in Florida had their child’s asthma inhaler instructions translated by a neighbor. The child was given the wrong number of puffs. After a trip to the ER, they found a nonprofit that provided free professional interpreters for LEP families. They now bring their child to every appointment with an interpreter. No more hospital visits. These aren’t rare cases. They’re common. But they’re also fixable.Final Thought: You Are Not Alone
If you’ve ever felt lost in a pharmacy, confused by a prescription, or afraid to ask for help because you didn’t speak English well-you’re not broken. The system is. But you have power. You have rights. And you have options. Speak up. Ask for an interpreter. Demand translated instructions. Use the teach-back method. Don’t let fear silence you. Your safety matters more than your discomfort. The next time you walk into a clinic or pharmacy, remember: you’re not asking for a favor. You’re claiming a right.Can I be charged for an interpreter at the hospital or pharmacy?
No. By federal law, healthcare providers that receive federal funding-like Medicare or Medicaid-must provide professional interpreters for free. You should never be asked to pay for interpretation services. If someone tries to charge you, ask to speak to a supervisor or file a complaint with the Office for Civil Rights.
What if my language isn’t commonly spoken, like Somali or Karen?
Even for less common languages, hospitals and large pharmacies are required to provide interpretation through phone or video services. These services cover over 200 languages. If you’re told they don’t have your language, ask them to connect you to their language services line immediately. Most can connect within 90 seconds.
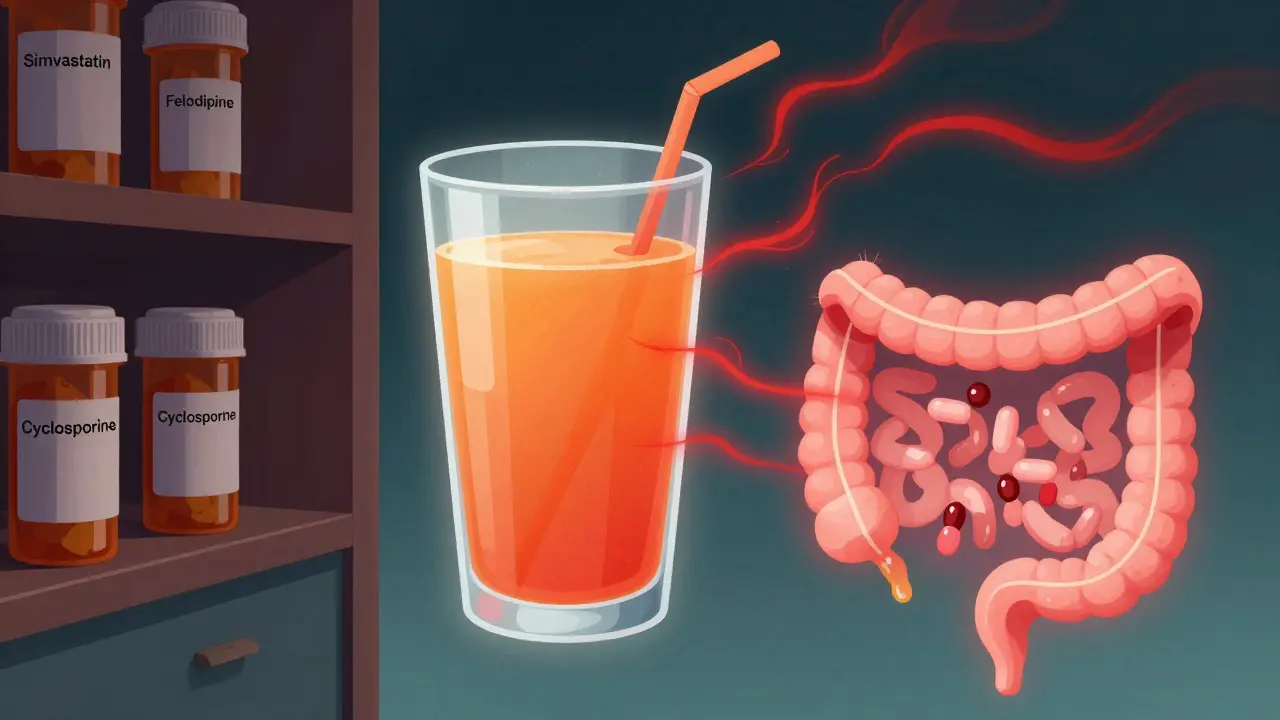
Is it okay to use Google Translate or a phone app for medication instructions?
No. Medical terms like "bid," "q.d.," or "take with meals" often translate incorrectly. Apps can’t understand context or dosage safety. A 2022 study found Google Translate misinterpreted 43% of common prescription terms. Always verify instructions with a professional interpreter or pharmacist-even if you use an app to help you prepare questions.
How do I know if my pharmacy provides translated labels?
Ask directly: "Can you print my prescription label in [your language]?" If they say no, ask if they can email or text it to you. If they still say no, ask to speak to the manager. You can also call the pharmacy’s corporate office or file a complaint with your state’s board of pharmacy. Many states track this data.
What should I bring to my appointment to make sure I understand my meds?
Bring a list of all your medications-including doses, times, and why you take them-in your language. Also bring any pill bottles or packaging. Ask for a professional interpreter before your appointment starts. If you’re unsure about something, say: "Can you show me how to take this?" and ask to watch someone demonstrate it.








Jenna Allison
January 23, 2026 AT 00:50Just had to call my pharmacist last week because the label said 'take one tablet q.d.' and I had no idea what that meant. Turned out it was 'once daily'-but why not just write it out? I asked for a Spanish version since my mom speaks it, and they emailed me a PDF within 10 minutes. Seriously, it’s not that hard. Just ask. Don’t assume they’ll know you need help.
Vatsal Patel
January 24, 2026 AT 00:05Ah yes, the great American healthcare circus. Where language is a luxury and survival is a privilege. We have AI translators that can identify cats in photos but can’t spell 'dosage' in Tagalog. The real tragedy? We all know this is fixable. But fixing it would mean admitting the system was never built for people like us. So we keep nodding, taking the wrong pills, and calling it 'culture'.
Helen Leite
January 25, 2026 AT 15:38THEY’RE LYING TO US 😱 I SAW A VIDEO WHERE A PHARMACY USED A ROBOT TO TRANSLATE INSULIN DOSES AND THE ROBOT SAID 'ONE DROP' BUT IT WAS ACTUALLY 10 UNITS 😭 WE’RE ALL BEING EXPERIMENTED ON. THE GOVERNMENT IS USING LANGUAGE BARRIERS TO CONTROL POPULATIONS. 🤫💊 #FreeTheLabels #PharmaMindControl
Shanta Blank
January 27, 2026 AT 08:26Oh sweet mercy. Another ‘woke’ healthcare manifesto. Let me guess-you also think people should stop eating sugar and start meditating while their blood pressure spikes? This isn’t about language. It’s about people refusing to learn English. You don’t need a translator when you’re holding a pill bottle with a picture of a heart and the word ‘TWO’ on it. Maybe stop blaming the system and start learning the language of your own damn body.
Tiffany Wagner
January 27, 2026 AT 20:41Karen Conlin
January 28, 2026 AT 07:09Let me tell you what happened when my cousin’s daughter got her first asthma inhaler. The pharmacist handed her the box in English. The kid, 8 years old, read it out loud to her mom in Hmong. The mom didn’t understand a word. So the pharmacist just said, ‘Here, watch me.’ And showed her how to press it, how many puffs, how to hold it. No interpreter. No app. Just presence. That’s what works. Not laws. Not apps. Human beings taking the time. You don’t need a degree to care. You just need to show up.
asa MNG
January 28, 2026 AT 11:46bro i tried using google translate for my blood pressure med and it said 'take with water' but it was 'take with food' and i got dizzy for 3 days 😭 i told my dr and he was like 'why didn't you ask?' i was scared to look dumb. we gotta do better. also i think the pharmacist was judging me. he had a mustache. 👨⚕️🙄
Chloe Hadland
January 30, 2026 AT 03:46Amelia Williams
January 31, 2026 AT 21:17I work at a community clinic and we started training all staff to say ‘What language do you prefer?’ at check-in. It’s not just about interpreters-it’s about dignity. One woman cried because no one had ever asked her before. We’ve cut med errors by 60% in 8 months. It’s not magic. It’s just basic human respect. And honestly? It’s cheaper than ER visits. Why aren’t we doing this everywhere?
Sharon Biggins
February 2, 2026 AT 00:06