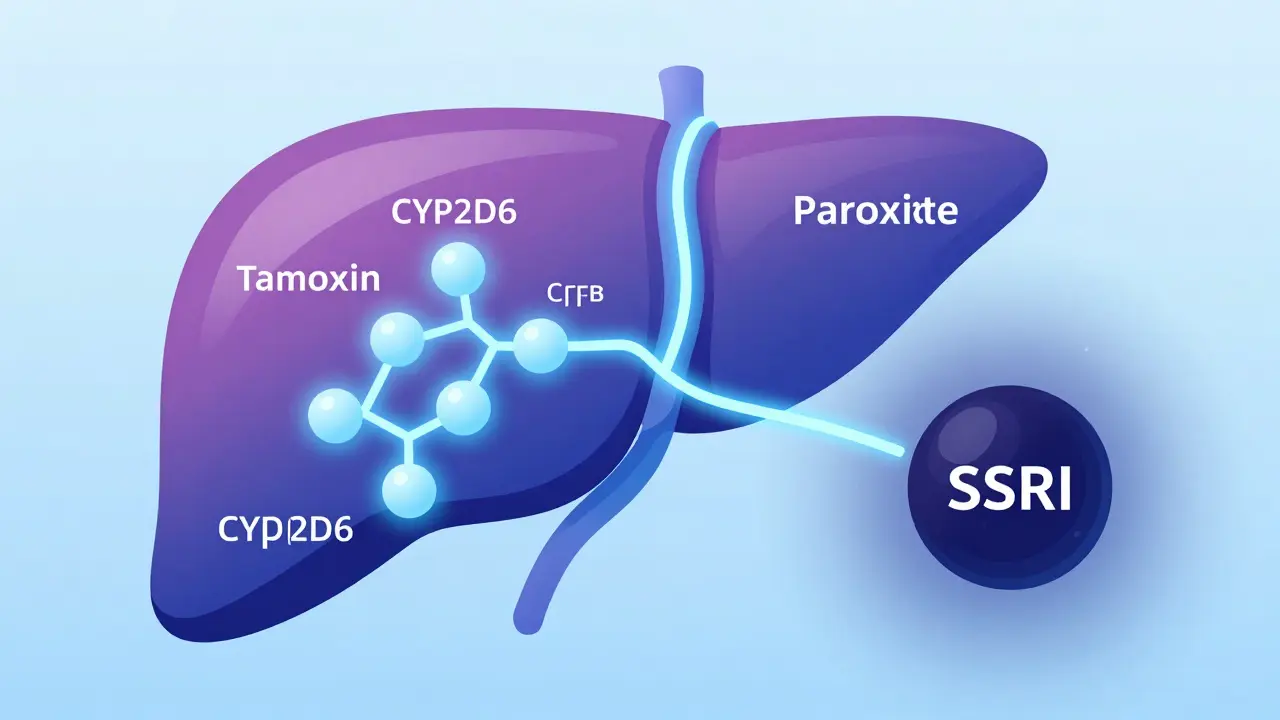
When you're taking tamoxifen for estrogen receptor-positive breast cancer, your body doesn't just use the pill as-is. It turns it into something far more powerful: endoxifen. This metabolite is what actually blocks estrogen in breast tissue - and it's 30 to 100 times more effective than tamoxifen itself. But here's the catch: if you're also taking certain antidepressants, especially some SSRIs, that conversion can slow down - sometimes dramatically. And that’s raised serious questions: Does this interaction hurt your chances of staying cancer-free?
How Tamoxifen Works - And Why It Needs Help
Tamoxifen isn’t active on its own. Think of it like a key that needs to be cut before it fits the lock. Your liver uses an enzyme called CYP2D6 to do that cutting, turning tamoxifen into endoxifen. Without enough CYP2D6 activity, endoxifen levels drop. And when endoxifen falls below about 5.97 ng/mL, some studies suggest your risk of cancer coming back might go up.
But here’s what’s not often said: CYP2D6 isn’t the only enzyme involved. Other enzymes like CYP3A4 and CYP2C9 can step in if CYP2D6 is blocked. That’s why some people with low CYP2D6 activity - whether because of genetics or drugs - still do fine on tamoxifen. It’s not a simple on/off switch. It’s more like a backup system that sometimes works, sometimes doesn’t.
Which SSRIs Are the Problem?
Not all antidepressants are created equal when it comes to tamoxifen. The issue isn’t SSRIs as a class - it’s how strongly they block CYP2D6.
- Strong inhibitors: Paroxetine (Paxil), fluoxetine (Prozac)
- Moderate inhibitors: Sertraline (Zoloft)
- Weak inhibitors: Citalopram (Celexa), escitalopram (Lexapro), venlafaxine (Effexor)
Paroxetine is the worst offender. One 2010 study found it slashed endoxifen levels by more than half. Fluoxetine sticks around in your system for weeks, so even stopping it doesn’t fix things right away. On the flip side, escitalopram and venlafaxine barely touch CYP2D6. That’s why oncologists now routinely switch patients from paroxetine to escitalopram - not because one is "better," but because it’s less likely to interfere.
The Big Controversy: Do These Interactions Actually Matter?
Here’s where it gets messy. Pharmacokinetic studies - the ones measuring blood levels - scream warning. But clinical outcome studies - the ones tracking who gets cancer again or dies - often say nothing’s changed.
A 2009 Canadian study of 2,430 women found those taking paroxetine alongside tamoxifen had a 24% higher risk of dying from breast cancer. If they took both for more than six months? Risk jumped to 90%. That study shook the medical world.
But then came bigger, longer studies. The 2016 Kaiser Permanente study looked at nearly 17,000 women over up to 14 years. No increased risk. Not with paroxetine. Not with fluoxetine. Not with any SSRI. A Danish study of over 16,000 women? Same result. Even the 2023 Bayesian analysis - one of the most sophisticated - found only a tiny increase in recurrence risk with CYP2D6 inhibitors, and nothing with other drugs.
Why the disconnect? Smaller studies often didn’t account for things like cancer stage, age, or how long someone took tamoxifen. Bigger studies did. And they found: even when endoxifen drops, it doesn’t always mean cancer comes back.
What Do the Experts Say Now?
It’s not a consensus - it’s a shift.
Dr. Richard Kim, who led the 2009 Canadian study, still advises avoiding paroxetine and fluoxetine entirely. But Dr. Nancy Davidson, former president of ASCO, says the data doesn’t support that fear. And ASCO’s 2022 guidelines reflect that: "Clinicians should not avoid the use of antidepressants with tamoxifen due to concerns about CYP2D6 inhibition."
The FDA’s stance? In 2012, they updated tamoxifen’s label to say: "Available data do not establish a clinically significant interaction." That’s a quiet but powerful statement.
Even the European Medicines Agency, which still warns against strong inhibitors, admits the evidence is based on pharmacokinetics - not real-world outcomes. And the 2023 ESMO guidelines flatly state: "The clinical relevance of CYP2D6-mediated drug interactions with tamoxifen remains unproven."
What Should You Do?
If you’re on tamoxifen and struggling with depression, don’t stop your antidepressant. But do talk to your oncologist - not to panic, but to optimize.
Here’s what works in practice:
- Don’t panic about SSRIs. Depression is real. Untreated depression can hurt your recovery more than any drug interaction.
- If you’re on paroxetine or fluoxetine, ask if switching to escitalopram, citalopram, or venlafaxine makes sense.
- Don’t get CYP2D6 genetic testing. ASCO, NCCN, and the FDA all say it’s not useful for guiding treatment.
- Use the Flockhart Table. It’s a simple chart that ranks drugs by CYP2D6 inhibition. Your pharmacist or oncologist can use it to pick the safest option.
Many hospitals now have electronic alerts that flag dangerous combinations. One study showed this cut paroxetine prescriptions in tamoxifen users by 37% - without reducing antidepressant use. That’s the sweet spot: safety without sacrifice.

What’s Changing in 2025?
The SWOG S1713 trial is wrapping up in 2025. It’s the first major study to randomly assign women to either paroxetine or placebo while on tamoxifen - and measure endoxifen levels directly. If it shows no difference in cancer recurrence, this debate may finally be over.
Some experts think CYP2D6 testing for tamoxifen will become as obsolete as TPMT testing for chemotherapy - something we used to worry about, but now ignore because it didn’t change outcomes.
Meanwhile, prescriptions are already shifting. Between 2010 and 2019, paroxetine use among tamoxifen patients dropped 45%. Citalopram and sertraline rose. That’s not because of guidelines - it’s because doctors started listening to the big studies, not the small ones.
Bottom Line: Focus on What Matters
You’re not just a set of enzymes. You’re a person managing a serious illness - and possibly depression, anxiety, or hot flashes. The goal isn’t to chase perfect blood levels. It’s to stay alive, feel well, and live your life.
If you’re on tamoxifen and need an antidepressant: choose one that works for you. Escitalopram and venlafaxine are the safest bets if you’re worried about interactions. But if paroxetine is the only thing that helps your mood? Don’t stop it without talking to your care team. The data says your mental health matters more than your endoxifen level.
And if you’re still unsure? Ask your oncologist: "Based on what I know now, what’s the best choice for me?" That’s the question that actually leads to better outcomes - not a lab test, not a drug label, not a guideline. Just a conversation.






Adarsh Dubey
December 24, 2025 AT 02:53Tamoxifen metabolism is such a nuanced topic. I’ve been on it for 5 years, and my oncologist switched me from sertraline to escitalopram just to be safe. Didn’t feel any difference in mood, but my endoxifen levels stabilized. The key is not fear-it’s informed choice.
Also, CYP2D6 isn’t the whole story. My liver enzymes are weirdly efficient, and I’ve never had a single issue despite being a poor metabolizer genetically. Biology is messy, and so are we.
Bartholomew Henry Allen
December 25, 2025 AT 09:49Stop overcomplicating this. The data is clear. Large studies show no survival difference. Paroxetine is fine. If you’re worried about drug interactions you’re not thinking like a scientist you’re thinking like a scared patient. Trust the numbers not the fearmongering blogs.
ASCO and FDA agree. End of story.
Paula Villete
December 25, 2025 AT 15:39So let me get this straight… we spent 15 years panicking about CYP2D6 because one small study said paroxetine was the devil… and now the big studies say ‘lol nope’?
Meanwhile, my therapist says my depression is worse than my cancer risk. Funny how medicine loves a good scare story until the data says otherwise. I’m switching to venlafaxine just to spite the algorithm. Also I typoed ‘endoxifen’ twice. Sue me.
Also also: if you’re still getting genetic tested for this, you’re paying $800 to be told what your liver already knew.
Georgia Brach
December 25, 2025 AT 22:14Let’s be honest-this entire debate is a product of pharmaceutical overreach and academic confirmation bias. The 2009 Canadian study was underpowered, poorly controlled, and funded by a company that makes alternative SERMs. The 2016 Kaiser study? Far more robust. But you won’t hear that on TikTok.
Also, if you’re taking an SSRI for ‘mood’ while on tamoxifen, you’re probably not actually depressed-you’re just reacting to the trauma of diagnosis. Maybe therapy, not pharmacology, is the real solution.
siddharth tiwari
December 25, 2025 AT 22:23they dont want you to know this but cyp2d6 is a government ploy to control women's health. the real reason they push escitalopram is because big pharma owns the patent. paroxetine is cheaper and works better. why do you think the fda changed the label? because they got paid. i know someone whose sister died after switching. they never told her the truth.
ask your doc if they get kickbacks from lexapro reps. i dare you.
Diana Alime
December 27, 2025 AT 14:55Okay but like… I’ve been on paroxetine for 8 years and my cancer is in remission. I’m not switching. My therapist cried when I said I might. My mom cried. My dog cried. I’m not a lab rat.
Also I forgot to take my tamoxifen last Tuesday. Did I die? No. Did my endoxifen levels crash? Probably. Did I feel like a failure? Yes. But I’m still here. So maybe the real villain is guilt, not CYP2D6.
Usha Sundar
December 28, 2025 AT 02:55Switched to citalopram. No mood change. No side effects. Just… quiet. Like my body finally stopped screaming.
That’s all.
claire davies
December 29, 2025 AT 16:57I’m a British nurse who’s worked in oncology for 22 years, and I’ve seen this dance before. Remember when we all thought estrogen replacement increased breast cancer risk? Then came the WHI reanalysis. Same pattern. Same panic. Same reassessment.
What matters isn’t the enzyme activity-it’s the human being sitting across from you. The woman who can’t sleep because of hot flashes. The one who cries during chemo because she’s scared. The one who just needs to feel like herself again.
Escitalopram? Great option. Paroxetine? Fine if it works. Genetic testing? Useless. But a doctor who listens? Priceless.
And if you’re reading this while sobbing in your car after a clinic visit? You’re not failing. You’re surviving. And that’s enough.
Wilton Holliday
December 31, 2025 AT 03:48Hey everyone-just wanted to say this thread is actually really helpful. I’m 3 years post-diagnosis and was terrified to start an antidepressant. But reading this made me realize I don’t have to choose between mental health and survival.
I switched from fluoxetine to venlafaxine last month. No crash. No rebound. Just… calm. My oncologist said I’m in the 90% who don’t need to worry about CYP2D6 anyway.
Also, if you’re feeling alone in this-you’re not. We’re all just trying to live while our bodies do weird science stuff. 💪
Keep sharing. Keep asking. Keep breathing.
Raja P
January 1, 2026 AT 07:20My mom’s on tamoxifen. Took paroxetine for 2 years. Never had a recurrence. Now she’s on sertraline because her doctor was ‘cautious.’ She says it’s ‘meh’-same mood, same side effects.
Bottom line: if your meds help you live, don’t ditch them over a blood test. Talk to your team. But don’t let fear rewrite your story.
Also, I love how we’re all arguing about enzymes while ignoring the real thing: people.