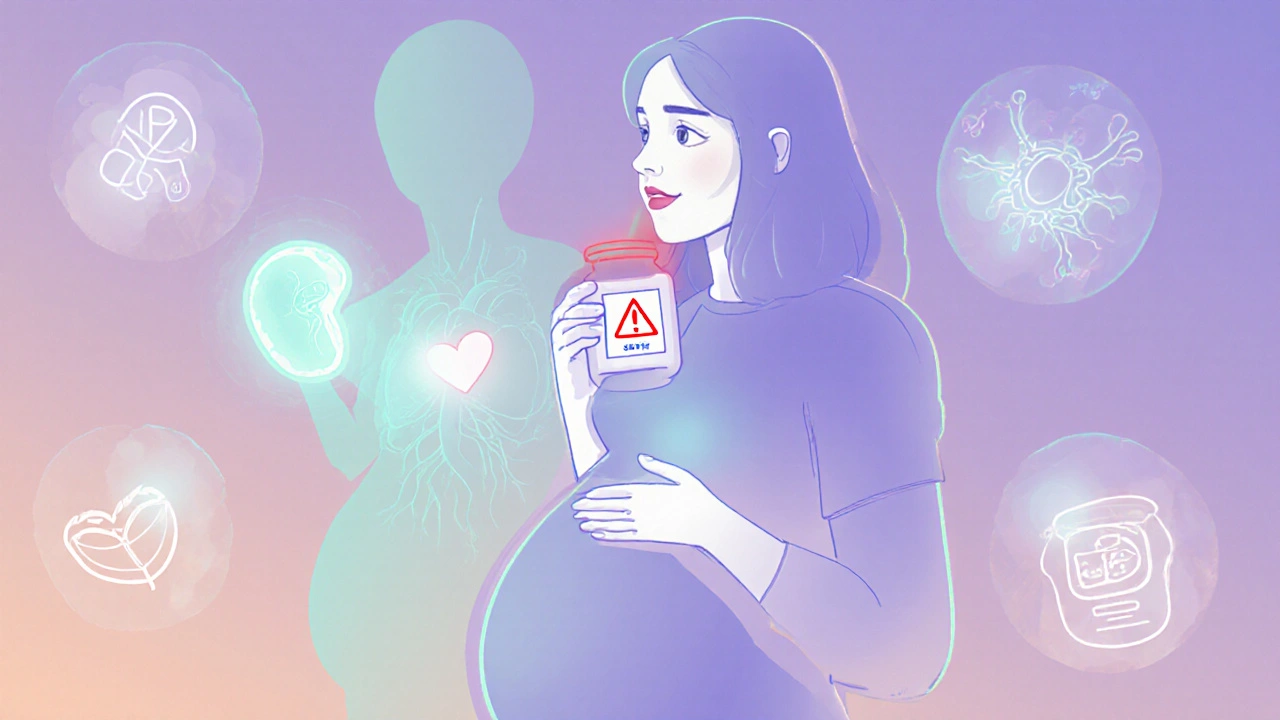
When you’re pregnant, every pill, supplement, or over-the-counter medicine feels like a gamble. You want to feel better - maybe you have a headache, nausea, or anxiety - but you’re terrified of hurting your baby. The truth is, teratogenic medications can cause real harm, but most drugs don’t. And the biggest risk isn’t always the medicine - it’s the untreated condition.
What Exactly Is a Teratogen?
A teratogen is any substance that can interfere with fetal development and lead to birth defects. It’s not just illegal drugs or experimental chemicals. Many common prescription and over-the-counter medicines fall into this category. The term comes from the Greek word teras, meaning monster - and that’s not an exaggeration. The thalidomide disaster in the 1950s and 60s showed the world what happens when a drug crosses the placenta unchecked. Around 10,000 babies were born with missing or shortened limbs after their mothers took it for morning sickness. That tragedy changed medicine forever. Today, we know that about 2-3% of all birth defects are linked to medications taken during pregnancy. That sounds low, but it’s still thousands of families affected every year. The key isn’t avoiding all drugs - it’s knowing which ones to avoid, when, and why.When Is the Baby Most at Risk?
Not all stages of pregnancy carry the same level of risk. The first trimester - especially weeks 3 to 8 after conception - is when the baby’s organs are forming. That’s the window when teratogens are most likely to cause major structural defects like heart problems, cleft lip, or missing limbs. After week 12, the risk of major physical deformities drops, but damage to brain development, hearing, vision, or organ function can still happen. In the second trimester, medications are more likely to affect growth or cause minor abnormalities. By the third trimester, the baby’s body is mostly built - but the brain is still wiring itself. That’s when drugs can cause problems like withdrawal symptoms, breathing issues, or long-term behavioral changes. Even a short course of certain antibiotics or painkillers late in pregnancy can have consequences.Medications with Proven Teratogenic Risks
Some drugs are known to be dangerous at any stage of pregnancy. Here are the ones you need to know:- Warfarin - Used to prevent blood clots, but it can cause fetal warfarin syndrome: underdeveloped nose, bone problems, eye damage, and intellectual disability. Risk is highest in the first trimester.
- Methotrexate - A drug for cancer and autoimmune diseases. It blocks folate, which is essential for neural tube development. Exposure in early pregnancy increases the risk of spina bifida and other defects by 10-20%.
- Carbamazepine - An anti-seizure medication linked to a 1% risk of neural tube defects. It also lowers vitamin K, which can cause dangerous bleeding in newborns.
- Factor Xa inhibitors - Drugs like rivaroxaban and apixaban. We don’t have enough human data, but animal studies show they cross the placenta. There’s no antidote if something goes wrong.
- Cannabis (THC) - Even if you think it’s “natural,” THC crosses the placenta. Studies show a 15-20% higher chance of low birth weight, 10-15% higher risk of preterm birth, and possible long-term effects on attention and learning. THC stays in breastmilk for up to six days.
These aren’t hypothetical risks. These are documented, repeated findings from thousands of pregnancies tracked over decades.
The Acetaminophen Controversy
This is where things get messy. Acetaminophen - Tylenol, paracetamol - is the go-to pain reliever for pregnant women. It’s been used for generations. But in recent years, some studies started linking long-term use to higher rates of ADHD and autism in children. The CDC flagged this as a potential concern. Then, in September 2025, the American College of Obstetricians and Gynecologists (ACOG) pushed back hard. ACOG said: “The conditions you treat with acetaminophen - fever, pain - are far more dangerous than any theoretical risk.” Untreated fever during pregnancy increases the risk of neural tube defects by 20-30%. Chronic pain can lead to depression, poor nutrition, and preterm labor. If you avoid acetaminophen because you’re scared, you might be putting your baby at greater risk. The truth? There’s no clear proof that acetaminophen causes autism or ADHD. But there’s strong proof that uncontrolled pain and fever hurt babies. So ACOG’s advice is simple: use it when needed, at the lowest dose for the shortest time. Don’t avoid it out of fear. Don’t overuse it out of convenience.How Medications Harm the Fetus
Not all damage comes from direct toxicity. Here are five ways drugs can affect your baby:- No effect - About 60-70% of medications don’t cross the placenta or don’t harm the baby. Many antibiotics, antacids, and allergy meds fall here.
- Direct damage - The drug attacks developing cells. Like methotrexate blocking folate.
- Indirect damage - The drug lowers your blood pressure so much that less oxygen and nutrients reach the placenta.
- Placental interference - Some drugs change how the placenta works, reducing nutrient flow.
- Uterine stimulation - Certain medications can trigger contractions, leading to preterm birth.
That’s why it’s not enough to just check a drug’s name. You need to understand how it works in your body - and how that affects your baby.
What You Should Do Before and During Pregnancy
You don’t need to panic. But you do need to be proactive.- Before you get pregnant - Talk to your doctor about every medication you take. That includes supplements, herbal remedies, and acne treatments. Some birth control pills, antidepressants, and blood pressure meds need to be switched out before conception.
- If you’re already pregnant - Don’t stop any medication without talking to your provider. Stopping seizure meds, insulin, or antidepressants can be more dangerous than keeping them.
- Use reliable sources - Don’t trust random blogs or Reddit threads. Use MotherToBaby, LactMed, or your pharmacist. These are science-backed, free services staffed by specialists who handle over 10,000 pregnancy medication questions every year.
- Check labels - The FDA no longer uses the old A, B, C, D, X categories. Now, prescription labels have detailed sections on pregnancy risks, clinical considerations, and data sources. Read them.
Here’s the hard truth: about 90% of pregnant women take at least one medication. Most are safe. But you can’t assume. You need to ask.

Why So Little Is Known
You might wonder: why don’t we know more? Why are so many drugs still a mystery? Because we can’t test them properly. Ethical rules prevent giving pregnant women new drugs in clinical trials just to see what happens. So 95% of what we know comes from watching what happens after the fact - case reports, registries, and observational studies. That’s why the data is messy. That’s why experts disagree. The FDA is trying to fix this with its Sentinel Initiative, tracking 10 million patient records to find patterns. But progress is slow. Right now, 70-80% of medications have inadequate safety data for pregnancy.What’s Changing in 2025
There’s hope on the horizon. Pharmacogenomics - testing how your genes affect how you process drugs - is starting to be used in pregnancy care. Imagine knowing, before you even take a pill, whether your body is likely to pass a dangerous amount to your baby. Experts predict this will improve personalized risk prediction by 30-40% in the next five years. Also, more doctors are working as teams. Your OB, your pharmacist, your mental health provider - they’re talking to each other. Nurses are being trained to flag potential risks before they become problems. And pregnancy registries, though underused, are growing. Over 50 now track medication exposures in real time.Bottom Line: Stay Informed, Not Afraid
Pregnancy isn’t a time to avoid all medicine. It’s a time to make smarter choices. The goal isn’t zero risk - it’s managing risk. A fever left untreated is more dangerous than acetaminophen. Uncontrolled seizures are more dangerous than carbamazepine. High blood pressure without treatment is more dangerous than labetalol. Talk to your provider. Don’t Google. Don’t rely on friends. Use trusted resources. Keep a list of everything you take - even ginger tea or melatonin. And remember: if you took a medication before you knew you were pregnant, don’t panic. Most exposures don’t cause harm. But do tell your doctor so they can monitor for any signs of concern. Your baby’s health matters. But so does yours. The best medicine isn’t the one with no side effects - it’s the one that keeps you alive, healthy, and calm enough to carry your baby to term.Can I take ibuprofen while pregnant?
Avoid ibuprofen after week 20 of pregnancy. It can cause low amniotic fluid and premature closure of a fetal heart vessel, which can lead to serious heart problems in the baby. Before week 20, occasional use may be okay under medical supervision, but acetaminophen is still the safer choice for pain relief.
Is it safe to take antidepressants during pregnancy?
For many women, yes - especially if stopping them would lead to severe depression or anxiety. SSRIs like sertraline and citalopram have the most safety data. Untreated depression raises the risk of preterm birth, low birth weight, and developmental delays. The benefits often outweigh the small potential risks. Always work with your doctor to choose the lowest effective dose.
What should I do if I took a risky medication before knowing I was pregnant?
Don’t panic. Most exposures don’t cause birth defects. Call your OB or a specialist at MotherToBaby (1-866-626-6847) to discuss what you took, when, and how much. They’ll assess your specific risk and may recommend a detailed ultrasound or genetic counseling. The fact that you’re asking means you’re already doing the right thing.
Are natural remedies safe during pregnancy?
Not necessarily. Many herbal supplements - like black cohosh, goldenseal, or dong quai - can trigger contractions or affect hormone levels. Even “natural” doesn’t mean safe. Ginger is generally okay for nausea, but high doses of vitamin A (from supplements, not food) can cause birth defects. Always check with your provider before taking anything not approved for pregnancy.
How can I find out if a medication is safe during pregnancy?
Use trusted sources: MotherToBaby.org, LactMed (from the National Library of Medicine), or your pharmacist. Avoid websites that sell supplements or rely on anecdotal stories. The FDA’s Pregnancy and Lactation Labeling Rule means prescription labels now include detailed risk information - read them. And never assume a drug is safe just because it’s sold over the counter.

Debanjan Banerjee
November 20, 2025 AT 15:35Just wanted to add that the MotherToBaby hotline is a godsend-my OB didn’t have time to explain carbamazepine risks, but their specialist walked me through the data in 10 minutes. No fluff, just facts. If you’re worried about a med, call them. Seriously. 1-866-626-6847. Saved my sanity.
Steve Harris
November 21, 2025 AT 00:00This is one of the clearest, most balanced takes I’ve read on pregnancy meds. Too many people treat it like a minefield, but the real danger is untreated illness. ACOG’s stance on acetaminophen? Spot on. Fear isn’t protection-it’s paralysis.
Michael Marrale
November 22, 2025 AT 09:44Wait… so you’re telling me the FDA and Big Pharma are hiding the truth about acetaminophen? I’ve seen videos-mothers who took Tylenol and their kids got autism. It’s not correlation, it’s causation. They’re covering it up because it’s profitable. Why else would they silence the studies? 🤔
David vaughan
November 23, 2025 AT 23:35I just want to say… thank you… for writing this… with such care… and clarity… I was terrified… after taking ibuprofen at 18 weeks… before I knew I was pregnant… and this… helped me breathe again… I’m not alone…
Cooper Long
November 25, 2025 AT 22:39Teratogenic risk assessment remains a deeply flawed domain due to systemic exclusion of pregnant populations from clinical trials. The reliance on observational data introduces significant confounding variables, particularly socioeconomic and behavioral confounders that are rarely adequately controlled. A more rigorous epidemiological framework is urgently needed.
Sheldon Bazinga
November 26, 2025 AT 17:18lol so now we're scared of tylenol but it's chill to take 500mg of ibuprofen like it's candy? dumbass culture. you wanna be a good mom? don't take shit. just suffer. that's what my grandma did. she had 7 kids and never took a pill. you're weak if you need meds.
Sandi Moon
November 27, 2025 AT 11:54Let us not forget: the thalidomide tragedy was not merely a medical failure-it was a societal collapse of oversight. Today, we have the same complacency wrapped in the velvet glove of ‘evidence-based’ euphemisms. The FDA’s Sentinel Initiative? A PR stunt. The real data is buried under layers of institutional cowardice.
Kartik Singhal
November 27, 2025 AT 17:38Bro, why are we even debating this? Everyone knows weed is fine. My cousin took THC daily and her kid’s now at Harvard. Also, if you’re stressed about meds, just drink coconut water and meditate. Science is for losers. 🌿🧠
Logan Romine
November 29, 2025 AT 16:11So we’re told to ‘stay informed, not afraid’… but the information is deliberately obscured, and the fear is weaponized. Is it really about safety-or about control? Who benefits when we’re too anxious to take a pill, but too confused to ask? 🤷♂️
Mark Kahn
November 30, 2025 AT 19:47You’re not alone. I was so scared after taking Zoloft before I knew I was pregnant. I cried for three days. Then I talked to my OB and realized-my mental health matters too. We’re not just vessels. We’re people. And taking care of ourselves IS taking care of our babies.
Daisy L
December 1, 2025 AT 01:05Okay but what about the fact that 90% of pregnant women take meds… and 99% of them have perfectly healthy babies? So why are we acting like every pill is a ticking bomb? I took Advil, melatonin, and caffeine like a boss-my kid’s now a 7-year-old ninja who eats kale and does cartwheels. Chill the f*** out.
Anne Nylander
December 1, 2025 AT 04:23OMG this post saved me!! I was gonna quit my antidepressants bc I was scared… but now I know it’s way worse to be depressed. I’m gonna talk to my doc tomorrow!! 💕
Franck Emma
December 2, 2025 AT 04:44I took four different meds before I knew I was pregnant. Now my kid has sensory issues. Coincidence? I don’t think so.
Noah Fitzsimmons
December 3, 2025 AT 04:04Oh wow, so you’re telling me the same people who told you to take folic acid are now telling you not to take Tylenol? What a surprise. You’re a gullible sheep if you believe anything the FDA says. I took ibuprofen at 16 weeks and my kid’s a genius. So there.
Eliza Oakes
December 4, 2025 AT 16:43And yet, no one talks about how the real teratogen is stress. The panic, the guilt, the endless googling-it’s worse than any pill. I took everything. I cried every day. My kid’s fine. But I’m not. And no one warned me about that.