When it comes to losing weight, most people have tried diets, exercise, and even weight-loss pills. But for many, the real problem isn’t willpower-it’s biology. Your body fights to hold onto fat, hormones signal hunger even when you’re full, and metabolism slows down just when you need it most. That’s where tirzepatide comes in. It doesn’t just suppress appetite. It rewires how your body manages energy, fat storage, and hunger signals. And it’s not just another GLP-1 drug like semaglutide. Tirzepatide is the first dual incretin therapy approved for weight loss, and its results are changing the game.
What Is Tirzepatide, Really?
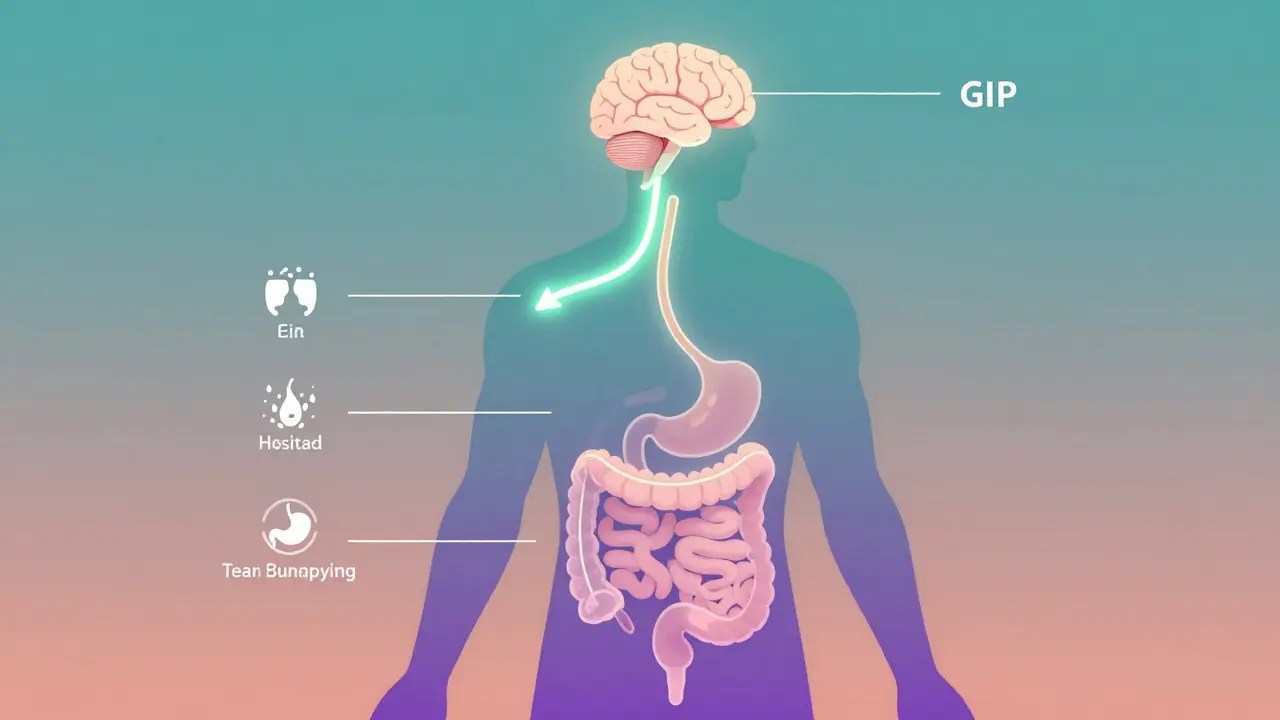
Tirzepatide is a synthetic molecule that mimics two natural hormones your body makes: GLP-1 and GIP. These are called incretins because they’re released by your gut after you eat, helping your pancreas release insulin and lowering blood sugar. But tirzepatide doesn’t stop there. It also talks directly to your brain-slowing down hunger, reducing cravings, and making food feel less rewarding.
It’s sold under two names: Mounjaro for type 2 diabetes and Zepbound for chronic weight management. The FDA approved Zepbound for weight loss in November 2023, making it the first dual-acting medication in this class. Unlike older drugs that only hit one target, tirzepatide hits two at once. That’s why it works better.
How much better? In clinical trials, people using the highest dose (15 mg weekly) lost an average of 22.4% of their body weight over 72 weeks. That’s not a few pounds. For someone weighing 250 pounds, that’s over 55 pounds gone. And unlike some weight-loss drugs, this isn’t just water loss. It’s fat loss-real, measurable, and sustained.
How Does It Actually Work?
Most weight-loss drugs focus on one thing: making you feel full. Tirzepatide does that, but it also does five other things at the same time:
- Slows stomach emptying, so you stay full longer
- Boosts insulin release only when blood sugar is high (low risk of low blood sugar)
- Reduces glucagon, the hormone that tells your liver to dump sugar
- Increases adiponectin, a fat-burning hormone that improves insulin sensitivity
- Directly reduces activity in brain areas that drive food cravings
Studies from Duke University show that activating both GLP-1 and GIP receptors together creates a synergy you can’t get with either one alone. It’s like turning up two volume knobs instead of one-the result is louder, clearer, and more effective.
What’s surprising? Even when people on tirzepatide ate the same number of calories as those on semaglutide, they still lost more weight. That points to another hidden effect: tirzepatide might actually help your body burn more calories at rest. Animal studies suggest it increases energy expenditure and improves how your muscles and fat tissue use fuel.
How Does It Compare to Semaglutide (Wegovy)?
Many people have heard of semaglutide-the drug behind Wegovy and Ozempic. It’s a GLP-1 agonist and was the gold standard for weight loss until tirzepatide came along.
In the SURMOUNT-1 trial, people on the highest dose of tirzepatide (15 mg) lost 22.5% of their body weight. Those on semaglutide (2.4 mg) lost 14.9%. That’s a 51% greater weight loss advantage for tirzepatide. And it wasn’t just a small edge-it was consistent across all doses.
Even more telling: tirzepatide users lost more visceral fat-the dangerous fat around organs-than semaglutide users, even when both groups lost the same amount of total weight. That matters because visceral fat is linked to heart disease, diabetes, and inflammation.
But here’s the catch: both drugs cause nausea, vomiting, and diarrhea. The difference? Tirzepatide’s side effects are slightly more common, especially at higher doses. But many users report that once they get past the first few weeks of dose escalation, the side effects fade.
What Are the Side Effects?
No drug is without trade-offs. Tirzepatide’s most common side effects are gastrointestinal:
- Nausea: 20-25% of users
- Diarrhea: 15-18%
- Vomiting: 7-10%
- Constipation: 10%
- Decreased appetite: 40%
These aren’t rare. About one in three people stop treatment because of them. But here’s what most people don’t tell you: side effects are usually worst during the first 4-8 weeks while your body adjusts to the dose. After that, most people feel better.
The FDA-approved dosing schedule is designed to minimize this. You start at 2.5 mg once a week for four weeks, then increase every four weeks until you hit your maintenance dose (5 mg, 10 mg, or 15 mg). Rushing this process increases side effects. Slowing it down-even going slower than recommended-can make a huge difference.
There’s also a black box warning for thyroid C-cell tumors in rodents. No cases have been seen in humans, but if you or a family member has a history of medullary thyroid cancer, you shouldn’t take it. Pancreatitis is another rare risk, but it’s no more common than with other GLP-1 drugs.
Who Is It For?
Zepbound is approved for adults with:
- A BMI of 30 or higher (obesity)
- A BMI of 27 or higher with at least one weight-related condition (like high blood pressure, type 2 diabetes, or sleep apnea)
It’s not for casual use. This isn’t a quick fix for someone who wants to lose 10 pounds before a wedding. It’s for people with obesity who’ve tried other methods and need a medical intervention that works at a biological level.
People with a history of pancreatitis, multiple endocrine neoplasia syndrome type 2, or severe gastrointestinal disorders should avoid it. Pregnant women shouldn’t take it either-there’s not enough data.
What Does Real-Life Use Look Like?
Reddit’s r/Mounjaro community has over 38,000 members sharing experiences. One user, u/HealthyJourney89, lost 58 pounds in six months on 15 mg. Another, u/StrugglingWithSideEffects, had to stop at 10 mg because nausea was too intense.
Drugs.com reviews show an average rating of 8.2 out of 10. About 76% of users report losing more than 10% of their body weight. But 32% quit because of side effects-mostly nausea and vomiting.
The key to success? Patience. Most people who stick with it past week 12 start seeing dramatic changes. One user said, “I didn’t feel hungry. I didn’t crave snacks. I just… stopped thinking about food.” That’s not just appetite suppression. That’s a reset.
Cost and Accessibility
The list price for a 4-week supply is over $1,000. But that’s not what most people pay. Thanks to Lilly’s co-pay assistance program, 89% of commercially insured patients pay under $100 a month. Medicare and Medicaid coverage varies, but many plans now cover Zepbound for eligible patients.
Insurance often requires proof of failed diet attempts, documentation of obesity-related conditions, or a referral from a specialist. Some primary care doctors prescribe it now, but endocrinologists and obesity specialists still handle most cases.
There’s also a patient support program through the Lilly Cares Foundation that helps with access and education. You don’t just get the drug-you get coaching on injection technique, diet tips, and how to manage side effects.

What Happens When You Stop?
This is the big question no one wants to talk about. Tirzepatide doesn’t cure obesity. It manages it. When people stop taking it, they tend to regain weight.
One extension study found that within six months of stopping, the average person regained 12-15% of the weight they lost. That’s not failure-it’s biology. Your body still wants to return to its old set point.
That’s why experts say tirzepatide should be seen like blood pressure or cholesterol medication: something you may need long-term. Some patients stay on it for years. Others use it to jump-start weight loss and then transition to lifestyle changes.
There’s no shame in needing help. Obesity is a chronic disease. You wouldn’t stop taking insulin for diabetes just because you lost weight. The same logic applies here.
The Future: What’s Next?
Tirzepatide isn’t the end-it’s the beginning. In October 2024, the FDA approved Zepbound for treating obstructive sleep apnea in adults with obesity. That’s huge. Sleep apnea isn’t just about snoring-it’s linked to heart failure, stroke, and early death. Tirzepatide doesn’t just help you lose weight; it helps fix the damage it caused.
Lilly is already testing a triple agonist called retatrutide, which targets GLP-1, GIP, and glucagon. Early results show 24.2% weight loss in just 24 weeks. That’s even more than tirzepatide.
Researchers are also studying its effects on non-alcoholic steatohepatitis (NASH), heart disease, and even Alzheimer’s. The science is clear: dual incretin therapy isn’t just a weight-loss drug. It’s a metabolic reset.
Final Thoughts
Tirzepatide isn’t magic. It doesn’t replace diet, exercise, or sleep. But for people who’ve struggled with weight loss despite doing everything right, it’s a lifeline. It doesn’t just help you lose weight-it helps you stop fighting your body every step of the way.
If you’re considering it, talk to a doctor who understands obesity as a medical condition-not a moral failing. Start low. Go slow. Give it time. And remember: the goal isn’t to be perfect. It’s to feel better, healthier, and in control.





Anu radha
December 16, 2025 AT 11:28I just started this and my stomach feels weird but I’m not hungry anymore. That’s magic to me.
Jane Wei
December 17, 2025 AT 00:40Been on it 3 months. Lost 42 lbs. Still get nauseous if I eat too fast. Just chew slow and drink water. Works.
Brooks Beveridge
December 17, 2025 AT 00:58This isn't about willpower. It's about biology screaming at us to survive while our world tells us to eat everything.
tirzepatide doesn't make you weak-it gives your body a chance to catch up with your mind.
You're not broken. You're just fighting an outdated system.
I've seen people cry because they finally feel like they can breathe again.
That's not a drug. That's a second chance.
And yeah, the side effects suck at first-but so does being trapped in your own body for years.
If this helps even one person stop hating their reflection, it's worth it.
We don't need more shame. We need more science that listens.
This isn't a quick fix. It's a quiet revolution.
And if you're scared to start? That's okay. Start small. Start slow.
You don't have to be perfect. You just have to show up.
I'm rooting for you. Even if we've never met.
❤️
Kaylee Esdale
December 18, 2025 AT 13:22My aunt lost 70 lbs on this and now she dances at family weddings again
I cried watching her
No more hiding in big clothes
No more avoiding photos
Just her. Happy. Light.
Side effects? Yeah she puked for weeks
But she said the silence in her head about food? Worth every second
This isn't vanity
This is freedom
Jody Patrick
December 18, 2025 AT 18:49Big Pharma pushing this to make you dependent. You don’t need drugs. Just quit eating junk.
Victoria Rogers
December 19, 2025 AT 05:44Why is this only approved in the US? Europe banned it because they know it’s a trap
They’re making us fat so we buy more meds
And the FDA? Paid off by Lilly
Read the animal studies
Thyroid tumors
They’re lying to us
You think this is science? It’s a money machine
Jonathan Morris
December 20, 2025 AT 04:29Contrary to popular belief, the 22.4% weight loss figure in SURMOUNT-1 is statistically significant (p<0.001) and replicable across subgroups. The claim that side effects diminish after 8 weeks is supported by longitudinal data from the SURMOUNT-2 trial (JAMA 2024). The thyroid C-cell tumor risk in rodents is not translatable to humans due to species-specific receptor expression. Regulatory agencies have consistently reaffirmed safety profiles. The narrative of corporate malfeasance is unfounded and distracts from legitimate clinical progress.
Philippa Skiadopoulou
December 20, 2025 AT 12:14Effective for weight loss yes but long-term data beyond two years remains limited. Monitoring for gastrointestinal intolerance and potential nutrient deficiencies is advised. Access remains inequitable due to cost and insurance barriers. A holistic approach including behavioral support is essential. This is a tool, not a cure.
Meghan O'Shaughnessy
December 21, 2025 AT 18:15I’m from India and we don’t even have access to this here
My cousin lost 60 lbs in the US on it
She’s alive again
But here? We’re lucky if we get metformin
This isn’t just medicine
It’s privilege
Marie Mee
December 22, 2025 AT 15:34They’re putting tracking chips in the needles you know
I read it on a forum
The government wants to control our eating habits
And the nausea? That’s the chemicals messing with your brain
Don’t trust them
They’re watching