More than one in three adults in the U.S. has metabolic syndrome-and most don’t even know it. This isn’t just one problem. It’s a cluster of five warning signs that, when they show up together, turn your body into a ticking time bomb for heart disease, stroke, and type 2 diabetes. You might have high blood pressure. Maybe your cholesterol looks off. Your waistline has crept up over the years. But if your doctor only treats each piece separately, you’re missing the bigger picture. Metabolic syndrome is the hidden link between all of them.
What Exactly Is Metabolic Syndrome?
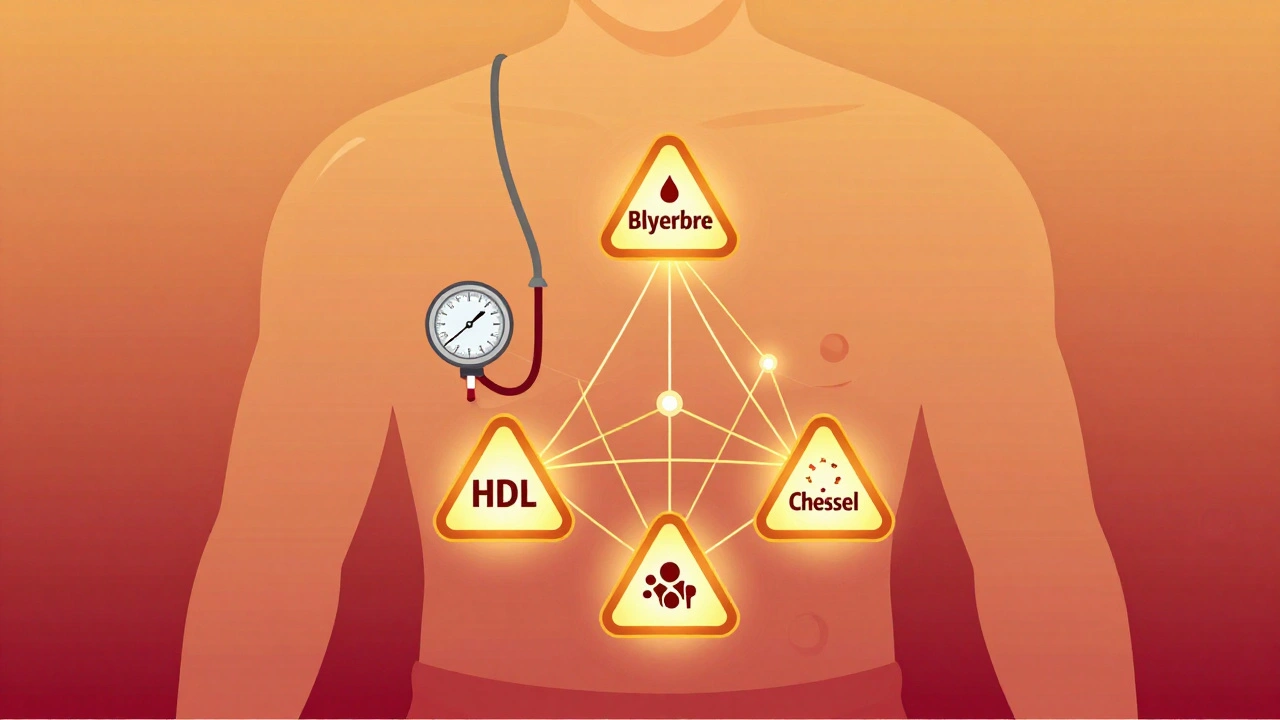
Metabolic syndrome isn’t a disease you can cure with a pill. It’s a pattern-a group of five specific health problems that happen at the same time. To be diagnosed, you need at least three of these five:
- Waist circumference over 40 inches (102 cm) for men, or 35 inches (88 cm) for women
- Triglycerides at 150 mg/dL or higher
- HDL cholesterol below 40 mg/dL for men, or 50 mg/dL for women
- Blood pressure at 130/85 mmHg or higher
- Fasting blood sugar of 100 mg/dL or higher
These numbers aren’t arbitrary. They’re based on decades of research from the American Heart Association and the National Institutes of Health. If you meet three or more of these criteria, your risk of having a heart attack or stroke doubles. Your chance of developing type 2 diabetes goes up five times.
What makes this different from just having high blood pressure or high cholesterol alone? It’s the way these factors feed into each other. Abdominal fat-especially the kind that wraps around your organs-isn’t just storage. It’s active tissue that releases inflammatory chemicals and fatty acids directly into your liver. That’s what triggers insulin resistance, the core problem behind the whole syndrome.
The Real Culprit: Insulin Resistance
Insulin is your body’s key to unlocking energy from food. When you eat, your pancreas releases insulin to tell your muscles and fat cells to take in glucose. But with metabolic syndrome, those cells stop listening. They become resistant. So your pancreas pumps out more insulin to compensate. That’s called hyperinsulinemia.
This isn’t just about sugar. High insulin levels mess with your blood vessels, raise your blood pressure, and make your liver churn out more triglycerides. It also lowers your good cholesterol (HDL). The result? A perfect storm for heart disease.
Dr. Scott M. Grundy, who helped set the official diagnostic guidelines, called insulin resistance the "common soil" where all these risk factors grow. That’s why treating just one piece-like lowering your blood pressure with medication-doesn’t fix the root cause. You’re putting out fires without turning off the gas.
Why Most People Miss It
Here’s the frustrating part: many people have three or four of these risk factors for years without ever being told they have metabolic syndrome. Primary care doctors often treat each condition in isolation. High blood pressure? Here’s a pill. High cholesterol? Take this statin. Elevated blood sugar? Let’s monitor that.
But if you’re not looking at the full picture, you’re missing the point. A 2022 survey on HealthUnlocked found that 68% of people with metabolic syndrome weren’t diagnosed until they had a heart event or were told they had prediabetes. By then, damage may already be done.
Reddit users in r/MetabolicSyndrome describe the same thing: "I had three red flags for five years. No one connected the dots." It’s not always the doctor’s fault. The system isn’t built to look at patterns. It’s built to treat symptoms.

Who’s Most at Risk?
Metabolic syndrome doesn’t pick favorites-but it does have preferences. The risk jumps sharply with age. About 20% of adults aged 20-39 have it. By age 60 and older, that number climbs to nearly 50%. Obesity is the biggest driver, especially abdominal fat. But it’s not just about weight.
Ethnicity matters too. In the U.S., Hispanic adults have the highest rate at 38.6%, followed by non-Hispanic whites at 34.2%, and non-Hispanic Blacks at 31.8%. Asian Americans develop metabolic syndrome at lower waist sizes-35 inches for men and 31 inches for women-because their bodies are more sensitive to fat around the midsection.
Women with polycystic ovary syndrome (PCOS) are especially vulnerable. Hormonal imbalances make insulin resistance worse, and weight loss becomes harder. Many women with PCOS are diagnosed with metabolic syndrome before they even realize they have PCOS.
Can It Be Reversed?
Yes. And not just managed-reversed.
The Diabetes Prevention Program, a landmark study backed by the NIH, showed that people who lost just 7% of their body weight through diet and 150 minutes of walking per week cut their risk of developing type 2 diabetes by 58%. That same lifestyle change reduced metabolic syndrome by 41% over 10 years.
One patient in the Mayo Clinic’s Integrated Metabolic Syndrome Program lost 22 pounds in six months. His triglycerides dropped from 280 to 110. His blood pressure fell from 145/92 to 120/78. His fasting glucose went from 112 to 88. He no longer met the criteria for metabolic syndrome. He didn’t take a single new medication.
Even more promising: the DiRECT trial in the UK found that 46% of people with type 2 diabetes and metabolic syndrome achieved remission after losing 15 kg or more through a structured, low-calorie diet. Their insulin sensitivity improved. Their liver fat dropped. Their blood pressure normalized. This isn’t just weight loss-it’s metabolic reset.

What Actually Works (And What Doesn’t)
There’s no magic pill for metabolic syndrome. Drugs can help with individual pieces-statins for cholesterol, ACE inhibitors for blood pressure, metformin for blood sugar-but none of them fix the underlying insulin resistance.
The only proven treatment? Lifestyle change. But not the vague "eat better and exercise" advice. You need structure:
- Diet: Cut added sugars and refined carbs. Focus on whole foods-vegetables, lean protein, healthy fats (olive oil, nuts, avocado), and fiber-rich grains. Women should aim for 1,200-1,500 calories a day; men, 1,500-1,800.
- Exercise: 150 minutes of moderate activity per week. That’s 30 minutes, five days a week. Brisk walking counts. You don’t need a gym.
- Weight loss: Losing 5-10% of your body weight can reverse at least two of the five risk factors.
- Sleep and stress: Poor sleep and chronic stress raise cortisol, which worsens insulin resistance. Aim for 7-8 hours a night.
Technology is helping. In January 2023, the FDA approved the first digital therapeutic for metabolic syndrome: DarioHealth’s Metabolic+ app. It uses continuous glucose monitoring and behavioral coaching. In a trial, users saw their waistlines shrink by 3.2 cm and their HbA1c drop by 0.6% in six months.
Community programs work too. The CDC’s National Diabetes Prevention Program uses trained lay health coaches-often from the same background as participants-to guide people through lifestyle changes. In Hispanic communities, these programs led to better weight loss than standard care.
The Bigger Picture
Metabolic syndrome isn’t just a personal health issue. It’s a public health crisis. In the U.S., it costs $219 billion a year in medical bills and another $143 billion in lost work. The number of people with it has jumped 35% since 2000. By 2030, nearly 40% of the world’s adults could have it.
But here’s the good news: it’s one of the most preventable conditions we have. Unlike genetic diseases or rare disorders, metabolic syndrome is shaped almost entirely by daily choices. Food. Movement. Sleep. Stress.
If you’re over 40, carry extra weight around your middle, or have one or two of the five risk factors, don’t wait for your doctor to connect the dots. Get your numbers checked. Measure your waist. Ask for a fasting glucose test. Don’t let your body send signals in silence.
You don’t need to be perfect. You just need to start. And you don’t have to do it alone. Support from a dietitian, a fitness coach, or even a peer group can make all the difference. The science is clear: reverse metabolic syndrome, and you reverse your risk of heart disease-before it’s too late.
Can you have metabolic syndrome without being overweight?
Yes, but it’s rare. Most people with metabolic syndrome have excess abdominal fat. However, some individuals with normal weight can still have insulin resistance due to genetics, sedentary habits, or poor diet. These cases are often called "TOFI"-thin on the outside, fat inside. The key is waist measurement, not just body weight. If your waist is over 35 inches (women) or 40 inches (men), you could still have metabolic syndrome even if your BMI is normal.
Does metabolic syndrome always lead to diabetes?
No, but it greatly increases the risk. About 75-80% of new type 2 diabetes cases in the U.S. are linked to metabolic syndrome. Having three or more of the five risk factors makes you five times more likely to develop diabetes within 10 years. But with lifestyle changes, you can prevent it. The Diabetes Prevention Program showed that 58% of high-risk individuals avoided diabetes through diet and exercise.
Is medication necessary to treat metabolic syndrome?
Not for the syndrome itself-there’s no drug approved to treat metabolic syndrome as a whole. But doctors may prescribe medications for individual components: statins for high cholesterol, blood pressure pills, or metformin for elevated blood sugar. These help manage symptoms but don’t fix insulin resistance. Lifestyle change remains the only treatment that can reverse the condition.
How long does it take to reverse metabolic syndrome?
Many people see improvements in as little as 6 months. Losing just 5-7% of body weight can lower triglycerides, improve HDL, and reduce blood pressure. Fasting glucose often drops within 3-4 months of cutting sugar and increasing activity. Complete reversal-no longer meeting the diagnostic criteria-is common within a year for those who stick with consistent lifestyle changes. The Mayo Clinic program reported 68% of participants reversed the syndrome after 12 months.
Can children get metabolic syndrome?
Yes, and it’s rising fast. With childhood obesity rates climbing, pediatric metabolic syndrome is no longer rare. Kids with a waist circumference above the 90th percentile for age and sex, along with high blood pressure, high triglycerides, low HDL, or elevated fasting glucose, can be diagnosed. Early intervention with diet, activity, and sleep improvements can prevent lifelong complications. The American Academy of Pediatrics now recommends screening obese children for metabolic syndrome starting at age 10.






Kyle Oksten
December 7, 2025 AT 05:37It’s wild how we treat symptoms like isolated bugs instead of seeing the whole system crashing. Insulin resistance isn’t just a number-it’s the quiet collapse of your metabolism, and no pill fixes that. The body doesn’t care about cholesterol numbers or BP readings. It cares about fuel, stress, and rest. We’ve turned medicine into a parts-replacement shop, but the engine’s still running on garbage.
Sam Mathew Cheriyan
December 8, 2025 AT 21:43lol so u mean the govnt and pharma r hiding the truth? i heard metabolic syndrome is just a way to sell more metformin and statins. my cousin in india eats rice 3x a day and is fine. maybe its all about sugar? or maybe its just stress? idk but i think they r lying.
Ernie Blevins
December 9, 2025 AT 19:23So let me get this straight. You’re saying if I just walk more and eat salad I can undo decades of bad habits? That’s cute. My dad had a heart attack at 58. He walked every day. Ate ‘healthy.’ Guess what? His insulin was still shot. This whole thing is a scam to make people feel guilty. You can’t out-walk a genetic predisposition.
Jennifer Anderson
December 10, 2025 AT 16:58Y’all are overcomplicating this. I was diagnosed with 3 outta 5 signs last year. Started walking my dog 20 mins a day, swapped soda for sparkling water, and cut out midnight snacks. Six months later? All numbers normal. No meds. Just consistency. You don’t need a PhD to fix this. You just need to start. And if you slip? Start again. No shame. 💪
Louis Llaine
December 12, 2025 AT 11:00Wow. Another ‘eat less, move more’ miracle cure. Did you also get the memo that this is the same advice they gave in 1987? And yet, the numbers keep climbing. Maybe the problem isn’t us. Maybe it’s the food system. Or the 80-hour workweeks. Or the fact that ‘healthy’ food costs 3x more than junk. But sure, let’s blame the person whose fridge is full of processed crap because they work two jobs and have no time.
Jane Quitain
December 12, 2025 AT 15:44OMG I just realized I’ve had 4 of these for YEARS and no one ever told me!! I thought I was just ‘a little slow’ or ‘stressed’. I’m gonna book a doctor’s appointment tomorrow!! 🙌 You’re all so brave for sharing this!! I feel seen!! 💕
Nancy Carlsen
December 12, 2025 AT 17:00This is the most hopeful thing I’ve read all year 🥹 I’m 47, had PCOS since 18, and thought I was doomed. But if 46% of people reversed diabetes with weight loss… maybe I can too? I’m starting with one walk a day. No pressure. Just progress. Thank you for writing this. 🌱❤️
Ted Rosenwasser
December 13, 2025 AT 19:45Let’s be real-the only reason this is ‘reversible’ is because the NIH funded studies that already assumed lifestyle change would work. The real issue is that we’ve pathologized normal human biology. You think your body was designed to survive on kale and Peloton? No. It was designed to survive famine. The ‘syndrome’ is just your physiology screaming against a culture of excess. The real cure? Stop pretending we’re not animals.
Helen Maples
December 14, 2025 AT 07:01Stop romanticizing ‘lifestyle change.’ It’s not a motivational quote. It’s hard, expensive, and often impossible without structural support. You need access to fresh food, safe spaces to walk, paid time off to sleep, and healthcare that doesn’t charge $200 for a fasting glucose test. If you’re telling someone to ‘just walk more’ while they live in a food desert and work two shifts, you’re not helping. You’re gaslighting.
Ashley Farmer
December 15, 2025 AT 19:43My sister was diagnosed last year. She’s 32, didn’t even know she had PCOS. She started a support group with three other women in her building. They cook together, walk after dinner, share recipes. No one’s perfect. But they show up. That’s the real magic-not the numbers, not the meds. It’s the community. You don’t have to fix everything alone.