Heart disease isn’t just something that happens to older people. It’s quietly building in many adults long before symptoms show up. The good news? Most cases are preventable. The bad news? Many people don’t know what’s actually putting them at risk. If you’re wondering whether your lifestyle, your age, or your family tree could be setting you up for trouble, you’re not alone. Let’s cut through the noise and lay out exactly what increases your risk - and what you can actually do about it.
Age Isn’t Just a Number - It’s a Major Factor
You can’t turn back time, but you can understand how time affects your heart. For men, the risk of heart disease starts climbing noticeably after age 45. For women, it’s around 55 - right around the time menopause hits. Why? Estrogen offers some protection before menopause. Once it drops, so does that shield. By age 70, about 70% of men and 60% of women will have some form of cardiovascular disease. That’s not inevitable - it’s just common.
Each decade after 40 adds roughly 10% to your lifetime risk. That doesn’t mean you’re doomed. It means you need to be more careful. A 40-year-old with high blood pressure and no exercise routine has a much higher risk than a 70-year-old who eats well, stays active, and keeps their numbers in check. Age doesn’t cause heart disease - it gives other risks more time to do damage.
Family History: Your Genetics Are Speaking
If your dad had a heart attack before he was 55, or your mom had one before 65, your risk jumps by 60% to 75%. That’s not a guess - it’s from the INTERHEART study, one of the largest ever done on heart disease. And if more than one close relative had early heart disease? Your risk climbs even higher.
Some people inherit specific gene mutations that make their cholesterol skyrocket. Familial hypercholesterolemia affects about 1 in 250 people globally. Left untreated, it can cause heart attacks in men by age 50 and women by age 60. That’s not rare. It’s genetic, and it’s dangerous.
But here’s the key: having a family history doesn’t mean you’re powerless. It means you need to be proactive. Get checked earlier. Talk to your doctor about cholesterol tests, blood pressure monitoring, and maybe even a calcium score scan. Knowing your risk early lets you act before it’s too late.
Smoking: The Single Most Preventable Killer
Smoking isn’t just bad for your lungs. It’s a direct attack on your arteries. Current smokers are 2 to 4 times more likely to develop coronary heart disease than non-smokers. Even smoking just 1 to 5 cigarettes a day raises your risk by 50%. That’s not a typo. Five cigarettes. That’s it.
In the U.S., smoking causes about 1 in every 4 deaths from heart disease. It damages the lining of your arteries, makes blood thicker and more likely to clot, lowers good cholesterol, and raises blood pressure. All at once.
Quitting changes everything. Within one year of quitting, your risk drops by half. After 15 years, it’s nearly the same as someone who never smoked. No medication, no surgery - just stopping. It’s the most powerful thing you can do for your heart, no matter your age.
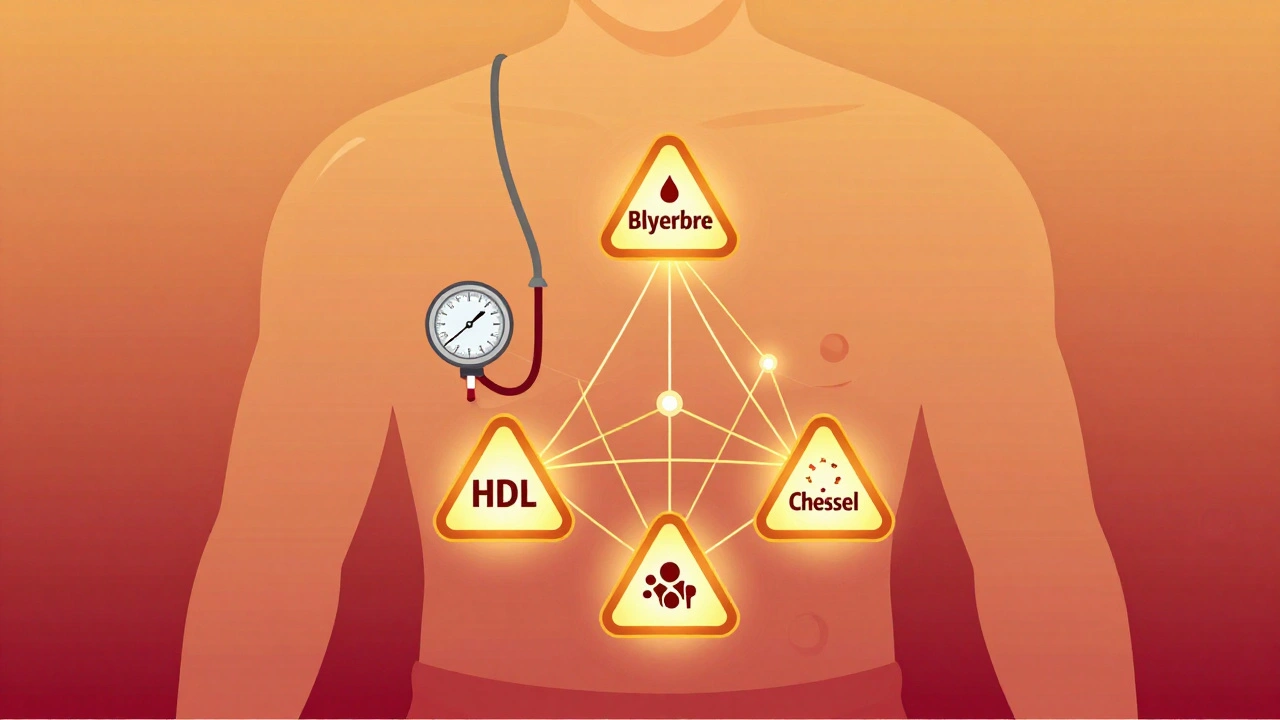
High Blood Pressure: The Silent Saboteur
One in two American adults has high blood pressure. That’s 116 million people. And most have no idea. That’s why it’s called the silent killer. Blood pressure above 130/80 mmHg starts damaging your arteries. Over time, that damage leads to heart attacks, strokes, and heart failure.
When uncontrolled, high blood pressure increases heart disease risk by 300% to 400%. It’s not just about the number. It’s about how long it’s been high. The longer it goes untreated, the more your heart has to work - and the more it weakens.
The SPRINT trial showed that lowering systolic pressure to under 120 (instead of the old 140 target) cut cardiovascular events by 25% in high-risk people. That’s huge. If you’ve been told your pressure is “a little high,” don’t wait. Start tracking it. Talk to your doctor. Lifestyle changes - salt reduction, exercise, weight loss - can often bring it down without meds. But if not, medication works. And it saves lives.

Cholesterol: Not All of It Is Bad
Ninety-four million Americans have LDL (“bad”) cholesterol above recommended levels. That’s 38% of the population. High LDL builds up in your arteries like rust in pipes. Over time, it forms plaques that can suddenly rupture and trigger a heart attack.
Having LDL above 190 mg/dL increases your risk by 50% compared to levels under 100. But it’s not just LDL. Low HDL (“good”) cholesterol also matters. HDL helps clean out the bad stuff. If your HDL is below 40 for men or 50 for women, your risk goes up.
Statins are the most studied and effective tool here. High-intensity statins (like atorvastatin or rosuvastatin) reduce heart attack risk by 25% to 35% in people who need them. The 2018 guidelines say if you’re over 40 with diabetes, high blood pressure, or a family history, you likely benefit from statins - even if your cholesterol isn’t “extremely” high. Talk to your doctor. Don’t fear the pill. Fear the plaque.
Diabetes: The Heart Disease Accelerator
Diabetes doesn’t just affect your blood sugar. It wrecks your blood vessels. People with diabetes are 2 to 4 times more likely to die from heart disease. And 68% of people with diabetes over 65 die from heart-related causes. That’s not coincidence. High blood sugar sticks to artery walls, causes inflammation, and speeds up plaque buildup.
It’s not enough to just control your sugar. New medications like SGLT2 inhibitors and GLP-1 receptor agonists don’t just lower glucose - they directly reduce heart attack and stroke risk by 14% to 26%. If you have diabetes, ask your doctor if one of these is right for you. It’s not just about insulin or metformin anymore.
Weight, Inactivity, and Diet: The Hidden Trio
Obesity, sitting too much, and eating poorly are the quiet engines behind most heart disease. The WHO links unhealthy diets to 11 million deaths globally each year. That’s more than smoking. Physical inactivity causes 6% of all coronary heart disease. And it’s not just about being overweight - it’s about what you eat and how little you move.
Diets high in processed foods, sugar, trans fats, and salt are the worst. They raise blood pressure, cholesterol, and inflammation. The CDC’s Sodium Reduction Program cut sodium intake by 14% in some communities - and saw a 5.8% drop in high blood pressure. That’s real. That’s measurable.
You don’t need a perfect diet. Start with small swaps: replace soda with water, walk 20 minutes a day, swap white bread for whole grain. Movement doesn’t have to be intense. Just consistent. The goal isn’t to run a marathon. It’s to keep your arteries clear.
Other Factors You Can’t Ignore
There are other risks that don’t get talked about enough. Air pollution? A 10 μg/m³ increase in PM2.5 particles raises heart disease death risk by 10% to 15%. That’s not just a city problem - it’s everywhere. Stress? Chronic stress raises cortisol and blood pressure. Sleep apnea? It doubles your risk of heart failure. Depression? It’s linked to a 60% higher risk of heart attack.
Social factors matter too. People in the lowest income brackets have 2 to 3 times higher heart disease death rates. Access to healthy food, safe places to walk, and quality healthcare all play a role. You can’t change your zip code, but you can ask your doctor about community programs - and push for better options.
What Should You Do Right Now?
Here’s the bottom line: 80% of premature heart disease is preventable. That’s not a slogan. That’s data from the American Heart Association. You don’t need to fix everything at once. Start with one thing.
- If you smoke - quit today. Call a quitline. Use nicotine patches. Ask for help. It’s the single biggest win.
- If your blood pressure is high - get it checked. Track it at home. Cut salt. Move more. Talk to your doctor about meds if needed.
- If you have diabetes - don’t just focus on sugar. Ask about heart-protective meds like SGLT2 inhibitors.
- If you have a family history - get screened early. Get a cholesterol panel. Ask about a calcium score.
- If you’re overweight or inactive - start walking. 20 minutes a day. Five days a week. That’s enough to make a difference.
There’s no magic pill. No miracle diet. Just consistent, smart choices. And they work. A 48-year-old man in a 2022 AHA case study cut his 10-year heart attack risk from 18.2% to 6.3% - just by quitting smoking, taking his meds, eating better, and walking daily. That’s not luck. That’s action.
Can you have heart disease even if you’re young?
Yes. While heart disease is more common in older adults, it can start early. Plaque builds up over decades. People in their 20s and 30s with obesity, diabetes, smoking, or family history can already have early artery damage. A calcium score scan can detect this before symptoms appear. Don’t assume youth protects you.
If my parents had heart disease, am I doomed?
No. Family history increases your risk, but it doesn’t decide your fate. People with strong family history who quit smoking, eat well, stay active, and take prescribed meds can reduce their risk to near-normal levels. Genetics loads the gun - lifestyle pulls the trigger. You control the trigger.
Is it too late to make a difference if I’m over 60?
Absolutely not. Studies show that even people over 70 who quit smoking, start walking, or get their blood pressure under control reduce their risk of heart attack and death. Your heart responds to change at any age. The sooner, better - but it’s never too late.
Do I need to take statins if I have a family history but normal cholesterol?
Maybe. The 2018 AHA/ACC guidelines say if you’re over 40 with a family history of early heart disease, you may still benefit from a statin - even with normal cholesterol. That’s because family history means you likely have other hidden risks: inflammation, genetics, or early plaque buildup. Talk to your doctor about a calcium score test. It can help decide.
Can stress really cause heart disease?
Chronic stress doesn’t cause heart disease directly, but it pushes up blood pressure, raises inflammation, and often leads to unhealthy habits like overeating, smoking, or skipping exercise. People with high stress and poor coping skills have a 20% to 30% higher risk. Managing stress - through sleep, movement, or therapy - is part of heart health.
Final Thought: Prevention Is a Practice, Not a One-Time Fix
Heart disease isn’t a mystery. We know what causes it. We know how to stop it. The problem isn’t lack of knowledge - it’s consistency. You don’t need to be perfect. You just need to keep showing up. Eat one more vegetable. Take the stairs. Skip the cigarette. Get your numbers checked. These aren’t grand gestures. They’re small, daily choices. And over time, they add up to a longer, healthier life.







Joseph Charles Colin
February 11, 2026 AT 10:36Let’s unpack the lipid dynamics here: LDL particle number (LDL-P) is a far superior predictor of CVD risk than LDL-C, especially in insulin-resistant phenotypes. ApoB is the gold-standard metric - every atherogenic particle carries one ApoB molecule. If your LDL-C is borderline-normal but your ApoB is >130 mg/dL, you’re still in high-risk territory. Most primary care docs still rely on LDL-C, which underestimates risk in metabolic syndrome. Get an NMR lipoprotein panel or an ApoB test. It’s not rocket science - it’s just not routinely ordered.
Same goes for hs-CRP. A value >2 mg/L indicates subclinical inflammation, which independently accelerates plaque vulnerability. Combine that with a calcium score >100, and you’ve got a perfect storm. Statin therapy isn’t optional here - it’s primary prevention with Level A evidence.
John Sonnenberg
February 12, 2026 AT 20:43Smoking is the single most destructive habit for your arteries - period. No debate. No nuance. No excuses. Two to four times the risk? That’s not a statistic - that’s a death sentence waiting to happen. And don’t tell me you ‘only smoke on weekends.’ One cigarette = 20 minutes of endothelial damage. You’re not a smoker who smokes occasionally - you’re a smoker who lies to yourself. Quit. Now. Or don’t. But don’t act surprised when your heart gives out at 52.
Joshua Smith
February 13, 2026 AT 00:51I really appreciate how this breaks down the science without fearmongering. I’ve been monitoring my BP at home since last year - it dropped from 138/88 to 122/76 just by cutting back on processed snacks and walking after dinner. Small changes add up. I also got my ApoB tested last month - it was 112, which my doc said was reassuring. I’m curious, though - for someone with a family history but no other risk factors, how often should you get a calcium scan? Every 5 years? Or is that overkill?
Jessica Klaar
February 14, 2026 AT 12:21Reading this made me think of my mom. She had her first heart scare at 61 - turned out she had silent ischemia. No chest pain. Just fatigue. She’s now on a statin, takes walks every morning, and refuses to eat white bread. I’ve started doing the same. It’s not about being perfect - it’s about showing up. My dad died of a heart attack at 58. I don’t want to repeat that story. So I’m listening. I’m learning. And I’m changing. Thank you for writing this - it felt like a conversation with someone who actually cares.
John Watts
February 14, 2026 AT 17:21You’re not too old. You’re not too late. You’re not too broken. That 70-year-old who started walking? He’s living proof. Your heart doesn’t care how old you are - it just wants you to move. One step. One vegetable. One less soda. That’s all it takes to begin healing. You don’t need a gym membership. You don’t need a personal trainer. You just need to stop waiting for tomorrow. Today is the day your future self thanks you for.
Ritteka Goyal
February 15, 2026 AT 23:38India has one of the highest rates of heart disease in the world - and we don’t even talk about it! People here eat ghee like it’s water, sit all day, and think chai fixes everything. My uncle had a stent at 49 - he smoked, ate biryani daily, and never checked his sugar. He thought heart disease was a ‘Western problem.’ Now he’s on 7 medications. I told him: your genes didn’t kill you - your habits did. If you’re Indian, you’re genetically predisposed to insulin resistance. That means you need to be twice as careful. No excuses. Eat less rice. Walk more. Stop lying to yourself.
Susan Kwan
February 16, 2026 AT 04:00Oh wow. A 12-page medical pamphlet disguised as a Reddit post. Congrats. You’ve successfully turned a simple message - ‘stop smoking and move more’ - into a 3000-word thesis. Do you get paid by the word? Or is this just your way of avoiding the fact that you’re 43 and still drink soda every day? Just quit. Walk. Sleep. Done. No need for calcium scores, ApoB panels, or SGLT2 inhibitors. Just stop being lazy.
Random Guy
February 17, 2026 AT 18:30bro i had a heart scan last year and they said my calcium score was 180. i was like ‘oh shit’ and then i just kept eating pizza. i’m 37. i’ve got time. also i smoke 3 cigarettes a day ‘for stress’ - that’s like 10% of a pack. how bad can it be? 🤔
Tasha Lake
February 18, 2026 AT 03:55Thank you for mentioning ApoB - most people don’t know it exists. But I’m curious: what about Lp(a)? It’s genetic, it’s not affected by diet or statins, and it’s a massive independent risk factor. If you have a family history of early heart disease and your Lp(a) is >50 mg/dL, you’re at high risk even if everything else looks normal. It’s under-tested, under-discussed, and under-treated. Most labs don’t even include it in standard panels. If you’re over 40 with a family history, ask for it. It could save your life.
Simon Critchley
February 19, 2026 AT 22:27Let me drop some truth bombs: the WHO’s sodium reduction program? Cute. The real problem? Industrial corn syrup, trans fats in fried chicken, and the fact that 80% of processed ‘low-fat’ foods are just sugar with a side of salt. We’ve been lied to for decades. ‘Low-fat’ doesn’t mean ‘heart-healthy’ - it means ‘corporate profit.’
And statins? They work - but only if you’re not eating a Big Mac every day. Lifestyle is the engine. Medication is the steering wheel. You need both. And yes - air pollution is a silent assassin. If you live in a city, wear an N95 on bad days. Your endothelium doesn’t care about your Instagram filter.
Karianne Jackson
February 20, 2026 AT 17:14I’m 52 and I just found out my cholesterol is high. I cried. I didn’t know. I thought I was fine because I don’t smoke and I walk my dog. But I eat a lot of cheese. A lot. Like, every day. I’m scared. I don’t want to die. What do I do now?
Tom Forwood
February 22, 2026 AT 04:04Love this. I’m a 41-year-old dad who just started walking 30 minutes after work. No fancy gear. Just sneakers and a playlist. My BP dropped 10 points in 6 weeks. I didn’t even think about it as ‘heart health’ - I just needed to get out of the house. My kid follows me now. We walk together. We talk. We don’t talk about heart disease. We just move. Sometimes that’s all you need. One step. Then another. Then another. That’s how you beat it.