Switching from a brand-name drug to a generic version seems simple: same active ingredient, lower price, same outcome. But what happens after six months? Or two years? For millions of people managing chronic conditions like high blood pressure, epilepsy, or diabetes, the real question isn’t whether generics work - it’s whether they keep working over the long haul.
Why the Switch Feels Safe - But Isn’t Always
The FDA requires generics to prove they’re bioequivalent to the brand-name drug. That means the amount of medicine absorbed into your bloodstream must fall between 80% and 125% of the original. Sounds tight, right? But here’s the catch: that range allows for a 45% difference in how much drug your body actually gets. For most people, that’s fine. For someone on warfarin, lithium, or seizure meds, even a small shift can mean the difference between control and crisis. A 2013 study in JAMA Internal Medicine found that patients with epilepsy who switched to a different generic version - even one approved as equivalent - saw their seizure control drop. Why? Because the pill looked different. Color, shape, size. These aren’t just cosmetic changes. For patients who take multiple pills daily, a change in appearance can trigger anxiety, confusion, or even the belief that the medicine isn’t working. That’s enough to make someone skip doses. And skipping doses over months or years? That’s how hospitalizations start.Manufacturing Matters More Than You Think
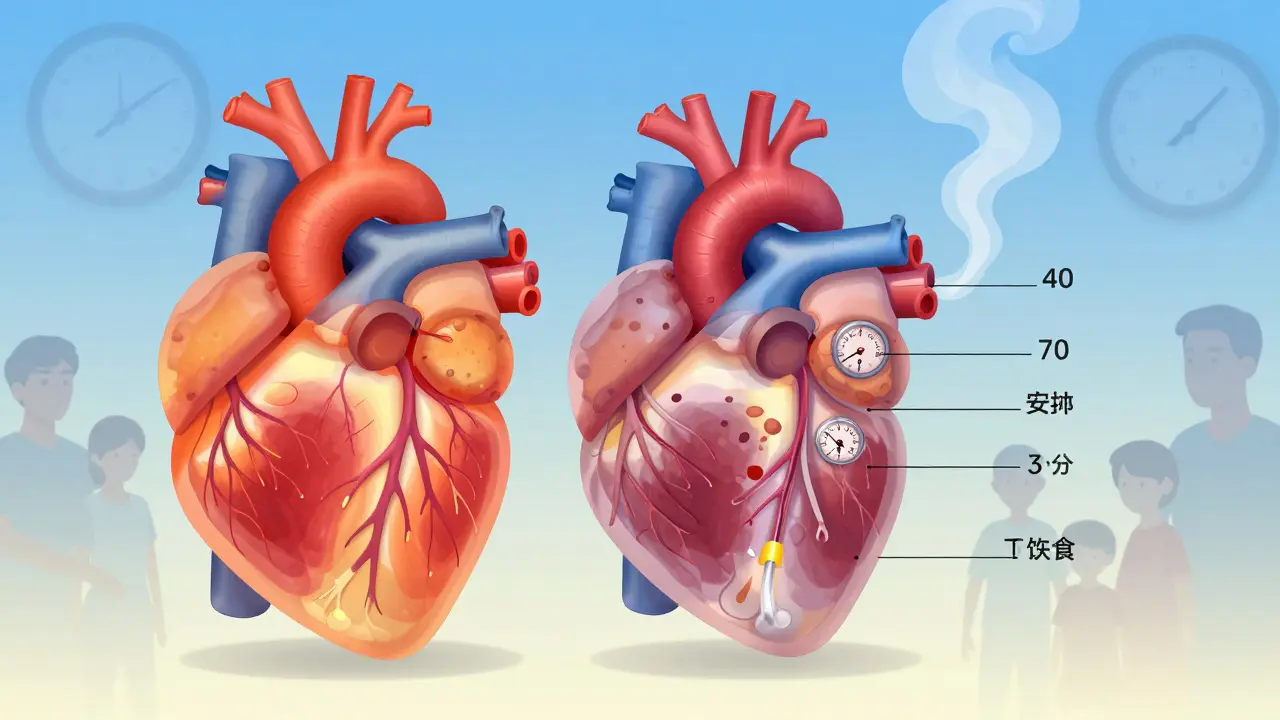
Not all generics are made the same. A 2021 study from Ohio State University found that generic drugs made in India had 27% more severe adverse events - including hospitalizations and deaths - than those made in the U.S., even when they were the same drug with the same active ingredient. This wasn’t about purity. It was about manufacturing consistency. Some factories use different binders, fillers, or coating processes. These aren’t active ingredients, but they affect how the drug dissolves in your gut. For a drug like metoprolol, which needs to release slowly over 24 hours, a bad coating can cause the whole dose to hit at once - leading to dizziness, low heart rate, or worse. One patient on PatientsLikeMe, who went by the name HeartWarrior42, switched from brand-name metoprolol to a generic and noticed his heart rate creeping up over 18 months. He ended up in the hospital twice with irregular rhythms. When he switched back to the brand, his rhythm stabilized. His doctor couldn’t explain it. The generic met the FDA’s bioequivalence rules. But the long-term effect? Clearly different.Adherence Isn’t About Cost - It’s About Trust
It’s often said that generics improve adherence because they’re cheaper. And yes, for statins, that’s true. A 2006 study showed 77% of people stayed on generic statins versus 71% on the brand. But that’s not the whole story. A 2019 survey of 1,200 patients with chronic illnesses found that 43% felt worse after switching to generics. Nearly 3 out of 10 stopped taking their meds altogether within six months. Why? Because trust breaks down. When your pharmacy switches your pill without telling you - and the new pill looks nothing like the old one - you start to wonder: Is this the same? Is it safe? Is it even working? One study from the University of Pittsburgh found that 61% of patients reported confusion or concern after a pill change. And 22% of them cut back on doses because they didn’t trust the new version. This isn’t just about psychology. It’s biology. If you take your blood pressure med inconsistently, your arteries suffer. If you skip your epilepsy drug, you risk a seizure. If you stop your diabetes med, your organs start to fail. The cost savings from generics vanish when you end up in the ER or hospital.
Who Gets Hurt the Most?
The people most at risk aren’t the ones taking one pill a day. They’re the ones on multiple meds, often older adults, with complex conditions. Take someone on warfarin, lisinopril, metformin, and levothyroxine. Each of these drugs has a narrow therapeutic index - meaning the difference between a good dose and a dangerous one is tiny. If each of those drugs gets switched to a different generic manufacturer every year - which happens often because insurance plans change their preferred brands - the risk of instability grows. A 2017 Canadian study tracked patients on generic blood pressure meds for a year. In the first month after switching, adverse events jumped by 8-14%. And they didn’t go back down. The longer patients stayed on the new generic, the more problems they had. The FDA says bioequivalence equals therapeutic equivalence. But real-world data says otherwise.What You Can Do to Protect Your Health
You don’t have to give up generics. But you do need to take control. Here’s how:- Ask your pharmacist - not just if it’s generic, but which manufacturer made it. Write it down. If the label changes, ask why.
- Don’t accept automatic switches - especially if you’re on a drug for epilepsy, thyroid disease, heart rhythm, or blood thinning. Tell your doctor you want to stay on the same generic brand. If your insurance forces a switch, ask for a prior authorization to keep your current one.
- Track your symptoms - keep a simple log: energy levels, heart rate, mood, sleep, any new side effects. If you notice a change after a switch, bring it to your doctor with your log.
- Request consistency - if you’ve been stable on a specific generic for over six months, ask your doctor to write “Dispense as written” or “Do not substitute” on your prescription. This legally prevents the pharmacy from switching you without permission.
Why the System Keeps Pushing Switches
Pharmacy benefit managers (PBMs) - the middlemen between insurers and pharmacies - push generics because they make money off the difference in price. Most Medicare Part D plans change their preferred generics every year. That means you might get one generic in January, another in July, and a third by December. Each switch carries risk. The American Heart Association recommends that patients on narrow therapeutic index drugs be kept on the same manufacturer for at least a year. But only 35% of U.S. health systems even track which generic manufacturer a patient is on in their records. That’s like driving a car without knowing what brand of gas you’re using - and hoping it doesn’t break down.
The Bigger Picture: Is This Sustainable?
Generics saved the U.S. healthcare system $1.67 trillion between 2008 and 2017. That’s huge. But a 2015 study in PharmacoEconomics found that 64% of the time, switching to generics didn’t lower overall healthcare costs - because more people ended up in the hospital. The savings on the drug were eaten up by emergency visits, lab tests, and hospital stays. The FDA is finally starting to respond. In 2023, they began requiring 36 months of stability data for generics used in chronic conditions - up from 24 months. The European Union now requires two years of real-world safety data before approving generics for long-term use. These are small steps. But they’re steps in the right direction. The truth? Generics are not all created equal. And for long-term health, consistency matters more than cost. If your medication keeps you alive and stable, don’t let a formulary change take that away.What’s Next?
The Institute for Safe Medication Practices wants to redefine what “therapeutic equivalence” means. They’re pushing for a new standard: any generic used for chronic conditions must prove it doesn’t worsen patient outcomes over 24 months. That proposal is under review by the FDA’s advisory committee and could become policy by 2025. Until then, the best defense is awareness. Know your drug. Know your manufacturer. Know your body. And if something feels off after a switch - speak up. Your long-term health depends on it.Are generic drugs really as safe as brand-name drugs in the long term?
For many medications, yes - generics perform just as well over time. But for drugs with a narrow therapeutic index - like those for epilepsy, thyroid disorders, or blood thinning - even small differences in how the drug is made can affect how your body responds over months or years. Studies show increased adverse events and lower adherence after switching, especially when the pill’s appearance changes or when you’re switched between different manufacturers.
Can switching to a generic cause my condition to get worse?
Yes, in some cases. Patients with epilepsy, heart rhythm disorders, and high blood pressure have reported worsening symptoms after switching to a different generic version - even when the FDA says it’s equivalent. This often happens because the inactive ingredients or coating differ, affecting how the drug is absorbed. In one study, patients on generic antihypertensives saw an 8-14% increase in adverse events in the first month after switching, and those issues persisted.
Why do pharmacies keep switching my generic medication?
Pharmacies switch generics because insurance plans and pharmacy benefit managers (PBMs) change which versions they cover to save money. Many plans switch preferred generics every year. You might get one brand in January and a completely different one in June. These switches are often automatic and not discussed with you - even though they can disrupt your treatment stability.
How can I stop my pharmacy from switching my generic drug?
Ask your doctor to write “Dispense as written” or “Do not substitute” on your prescription. This legally prevents the pharmacy from switching your medication without your doctor’s approval. You can also ask your pharmacist which manufacturer makes your current generic and request to stay on that version. Keep a record of the manufacturer name - if it changes, speak up.
Should I avoid generics altogether?
No. For most people, especially those on statins or common antibiotics, generics are safe, effective, and save money. But if you’re on a chronic condition medication - especially one with a narrow therapeutic index - consistency matters. Stick with the same manufacturer if it’s working. Don’t let a formulary change force you into an unknown. Talk to your doctor before any switch.





Grant Hurley
December 2, 2025 AT 12:20i switched my blood pressure med to generic last year and honestly? my heart started acting up. not dramatic, just weird fluttery stuff. i thought it was stress until i checked the pill - same name, different color. switched back to the brand and boom, normal again. doc didn’t believe me till i showed him the bottle change.
Lucinda Bresnehan
December 2, 2025 AT 22:03as a nurse who’s seen this happen over and over, i can’t stress this enough: it’s not about the active ingredient, it’s about the fillers. some generics use different binders that change how fast the drug dissolves. for someone on levothyroxine? that’s a nightmare. one patient lost 20 lbs in 3 months because her thyroid med was absorbed too fast. she thought she was just ‘eating right.’
always ask for the manufacturer name. write it down. if it changes, call your doctor. it’s not paranoia - it’s pharmacology.
ANN JACOBS
December 3, 2025 AT 23:01While I appreciate the sentiment and the empirical data presented, I must respectfully assert that the underlying assumption - that bioequivalence equates to therapeutic equivalence - is fundamentally flawed when applied to chronic, high-risk pharmacological regimens. The human organism is not a test tube; it is a dynamic, adaptive, and highly sensitive system. Variations in excipients, dissolution profiles, and even gastrointestinal pH interactions can precipitate cascading physiological consequences over time, particularly in geriatric populations with polypharmacy. The FDA’s regulatory framework, while well-intentioned, remains anchored in 20th-century pharmacokinetic models that fail to account for longitudinal patient-reported outcomes. This is not an indictment of generics per se, but rather a call for a paradigm shift toward outcome-based equivalence criteria - not merely concentration-based thresholds.
Nnaemeka Kingsley
December 5, 2025 AT 12:17man i never thought about this. i take my meds and never check who made them. but now i see - if your pill looks different, you start doubting it. and if you doubt it, you skip it. and then you end up in hospital. that’s crazy. i’m gonna ask my pharmacist next time. thanks for the heads up.
Kshitij Shah
December 5, 2025 AT 17:31so let me get this straight - the FDA says it’s the same, but if your pill changes color, your body goes ‘nah’? and the system doesn’t care because the insurance company saves 50 cents? wow. america. you can’t make this up.
Jaswinder Singh
December 5, 2025 AT 21:51you people are acting like this is a surprise. i’ve been on warfarin for 12 years. every time they switch my generic, i get a nosebleed or a headache. i’ve been screaming at my doctor for years. nobody listens. they just say ‘it’s the same chemical.’ yeah, and your car has the same engine as a tractor - doesn’t mean you can drive it on the highway.
stop being polite. demand your brand. if they won’t give it, go to a different pharmacy. or go to canada. at least they care about you there.
Jeremy Butler
December 6, 2025 AT 02:57It is a profound irony that a system predicated on cost-efficiency has become the very architect of its own systemic failure. The commodification of pharmaceuticals has reduced human physiology to a line item on a spreadsheet. The pharmacological integrity of the individual - their neurochemical equilibrium, their endocrine stability, their very capacity for homeostasis - is sacrificed on the altar of fiscal prudence. The FDA’s bioequivalence standards, while mathematically elegant, are ethically bankrupt when they fail to account for the lived experience of chronic illness. One cannot quantify trust. One cannot measure fear. And yet, these are the very variables that determine therapeutic success.
Courtney Co
December 7, 2025 AT 23:44i switched to generic lisinopril and started crying for no reason. like, full-on sobbing at the grocery store. i thought i was depressed. turns out my blood pressure was crashing. my doctor said it was ‘just hormones.’ i didn’t believe him. i went back to the brand and i haven’t cried since. why is this so hard to understand? my body knows the difference. why don’t you?
Shashank Vira
December 9, 2025 AT 21:51It is rather elementary, isn’t it? The very notion that a drug’s efficacy can be reduced to a narrow statistical range - 80% to 125% - while ignoring the subtle, non-linear pharmacodynamic responses of the human organism is a hallmark of reductionist scientism. One does not equate a Stradivarius with a factory-made violin merely because both produce A440. The timbre, the resonance, the soul - these are lost in translation. And yet, we allow corporate formularies to dictate the very rhythm of our lives. How tragic. How… bourgeois.
Irving Steinberg
December 9, 2025 AT 22:35bro just ask your doc to write ‘do not substitute’ on the scrip 😎 it’s literally that easy. i’ve been on the same generic for 3 years now because i told my pharmacist ‘if you switch me i’m gonna throw a fit’ 🤷♂️ and they didn’t. now i just check the pill color every time i get it. if it’s different? i call the doctor. done. problem solved. why is this so hard?
Lydia Zhang
December 11, 2025 AT 22:13my pharmacy switched me twice last year. i didn’t notice until i ran out and got a different one. i felt fine. maybe it’s just me.
Kay Lam
December 12, 2025 AT 07:00for anyone reading this who’s been told ‘it’s just a pill’ - please hear me. your body remembers. if you’ve been stable on a specific generic for six months, don’t let a formulary change steal that stability. write down the manufacturer name. take a photo of the pill. keep a journal. if you feel off - fatigue, dizziness, anxiety - don’t dismiss it as ‘getting older’ or ‘stress.’ it could be the coating on your pill. your doctor might not know this stuff. you’re the expert on your own body. speak up. keep track. be your own advocate. you deserve to feel safe in your own skin.
Matt Dean
December 14, 2025 AT 01:30if you’re complaining about generic pills, you’re probably the same person who buys organic kale and pays $12 for avocado toast. get over it. generics are fine. if you can’t handle a different color pill, maybe you need therapy, not a new prescription.