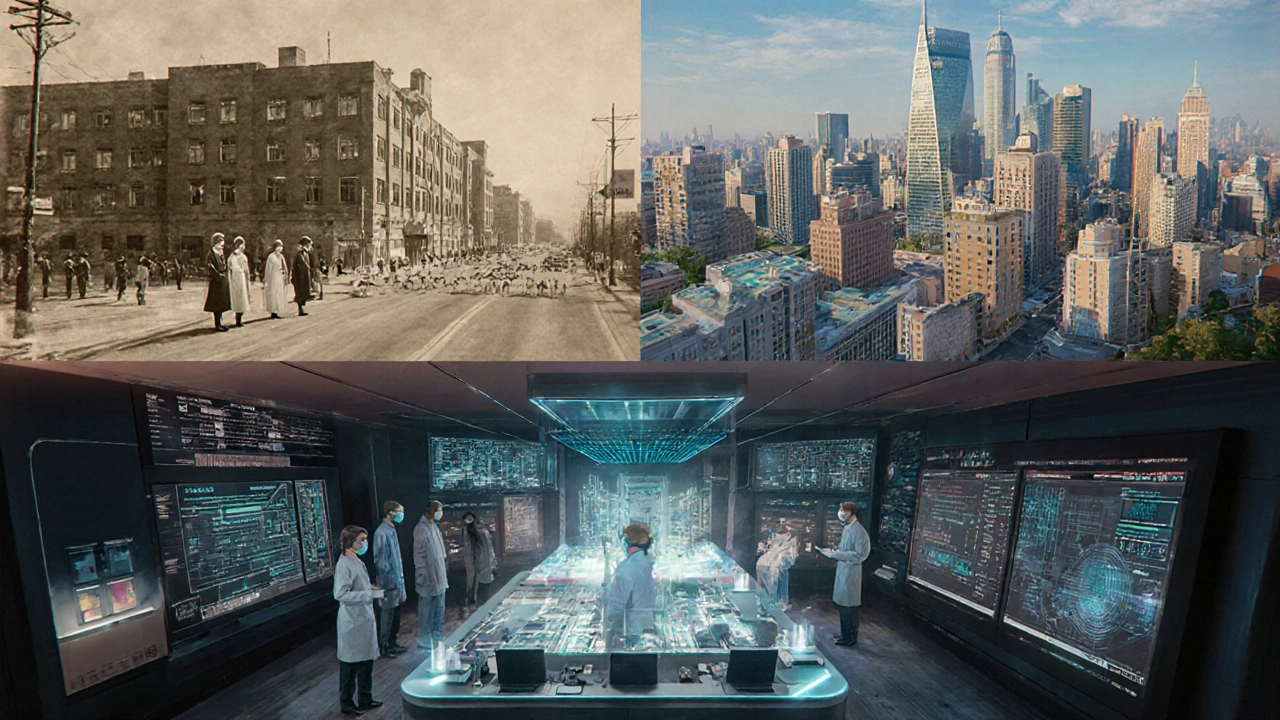
When a new wave of influenza pandemic spreads globally, it revives memories of past health crises and forces societies to re‑evaluate old playbooks, the world watches closely. In 2025, clusters of a novel H3N2 strain have been reported across Southeast Asia and are now appearing in Australia and Europe. The urgency is real, but the playbook isn’t blank - decades of data, vaccine tweaks, and policy shifts offer a clear roadmap.
Quick takeaways
- Robust surveillance caught the first 2025 cases within weeks, echoing lessons from the 2009 H1N1 response.
- Rapid vaccine platform updates cut production lag from 6 months (1918) to under 8 weeks.
- Clear, consistent messaging reduced vaccine hesitancy compared with the 1957 Asian flu.
- Combining masks, ventilation, and targeted school closures proved more effective than any single measure.
- International data sharing through the WHO’s Pandemic Hub accelerated drug‑level decisions.
Where we stand today
Australia’s National Influenza Surveillance System logged a 2.3% positivity rate in the first two weeks of September, double the seasonal average. Meanwhile, the World Health Organization coordinates global alerts, shares sequencing data, and recommends vaccine strain updates has already issued an interim vaccine recommendation for the H3N2 variant.
Unlike the 1918 Spanish flu, which had no coordinated response, today’s health agencies can deploy antivirals, issue travel advisories, and roll out digital exposure‑notification apps within days. Yet, challenges remain: production bottlenecks for egg‑based vaccines, uneven public trust, and the need for rapid‑scale testing.
Historical pandemics at a glance
| Year | Virus subtype | Estimated global deaths | Vaccine status | Primary public‑health tools |
|---|---|---|---|---|
| 1918 | H1N1 (Spanish flu) | 50‑100 million | None - vaccines unavailable | Quarantines, public‑space closures |
| 1957 | H2N2 (Asian flu) | 1‑2 million | Early inactivated vaccine, limited rollout | Travel restrictions, school closures |
| 1968 | H3N2 (Hong Kong flu) | 1‑4 million | Improved egg‑based vaccine, broader distribution | Mask mandates, public education |
| 2009 | H1N1 (Swine flu) | ~284,000 | Cell‑based vaccine, rapid scale‑up | Online surveillance, antiviral stockpiles |
| 2025 | H3N2 (novel strain) | Projected 0.5‑1 million (still unfolding) | mRNA‑platform vaccine in trial, expedited approval pathways | Real‑time genomic sequencing, digital exposure alerts |
What history taught us
Each pandemic sharpened a different part of the response puzzle. Pulling the threads together reveals four pillars that consistently determine outcomes.
1. Early, granular surveillance
The Centers for Disease Control and Prevention runs the FluView platform, aggregating lab reports, hospital admissions, and death certificates in near real‑time proved decisive in 2009, shortening the peak by weeks. Today’s genomic sequencing pipelines can flag a new strain within 48 hours, a speed unimaginable in 1918.
Lesson: invest in decentralized testing labs and open‑source data dashboards. The faster you see a spike, the faster you can mobilize resources.
2. Flexible vaccine platforms
Egg‑based production dominated the 20th‑century pandemics, causing months‑long delays. The shift to cell‑based and mRNA technologies, accelerated after the COVID‑19 crisis, trimmed the lead time to under two months for the 2025 strain.
Lesson: governments should pre‑fund platform‑agnostic facilities and maintain “vaccine banks” of ready‑to‑fill genetic templates.
3. Trust‑worthy communication
Public fatigue during the 1957 Asian flu stemmed from inconsistent messaging, leading to low vaccine uptake. In contrast, the coordinated WHO‑CDC briefings during the 2009 outbreak used clear visual aids and multilingual updates, achieving >60% coverage in high‑risk groups.
Lesson: consistency, transparency, and community‑level spokespersons (e.g., local GP champions) cut through misinformation.
4. Layered non‑pharmaceutical interventions (NPIs)
Mask mandates alone saved few lives in 1918, but when combined with school closures and ventilation upgrades in 1968, mortality fell dramatically. The 2025 response pairs rapid antigen testing with targeted indoor‑air quality standards, a synergy that models predict can reduce transmission by up to 45%.
Lesson: no single measure is a silver bullet; a toolbox approach adapts to local risk levels.

Practical steps for you right now
Even if you’re not a health official, a few actions can protect you and your community.
- Get vaccinated as soon as the updated H3N2 shot becomes available. The mRNA version offers >70% effectiveness against severe disease.
- Keep a 30‑day supply of antiviral medication such as oseltamivir, prescribed for post‑exposure prophylaxis if you belong to a high‑risk group.
- Improve indoor ventilation - open windows, use HEPA filters, and monitor CO₂ levels to stay below 800ppm.
- Use rapid antigen tests if you develop any flu‑like symptoms, especially before attending gatherings.
- Follow local health‑authority alerts via official apps or SMS services; they often include exposure notifications linked to the WHO’s Pandemic Hub.
Guidance for policymakers
To translate historical lessons into modern policy, leaders should focus on four actionable domains.
- Funding flexible vaccine R&D: grant mechanisms that reward platform adaptability, not just a single product line.
- Expanding real‑time surveillance networks: partner with universities to deploy wastewater monitoring and syndromic surveillance in schools.
- Building public‑trust pipelines: anchor briefings in data visualizations, involve community influencers, and pre‑approve multilingual messaging templates.
- Creating NPI rapid‑response toolkits: stockpiling masks, air‑purifiers, and clear protocols for temporary school closures with minimal disruption.
Looking ahead - the next 10 years
Experts project that climate change will broaden the geographic range of avian influenza reservoirs, increasing the odds of another pandemic. The key to staying ahead lies in integrating lessons from every past wave.
Future technologies - such as universal flu vaccines targeting conserved hemagglutinin stalk regions, AI‑driven outbreak prediction, and decentralized manufacturing - will only be effective if the foundational pillars of surveillance, communication, and trust remain strong.
Frequently Asked Questions
Why is the 2025 influenza strain considered more dangerous than the 2009 H1N1?
The 2025 H3N2 variant shows a higher basic reproduction number (R₀≈2.1) compared with 1.4 for the 2009 H1N1, meaning it spreads faster. Early data also suggest a higher rate of severe pneumonia in older adults, which pushes mortality projections upward.
How do modern vaccines cut production time compared to the 1918 Spanish flu?
Today’s mRNA platforms use synthetic nucleic acids that can be assembled in weeks, whereas 1918 relied on egg‑based methods that required weeks of virus adaptation and hundreds of egg‑laden incubators, stretching production to six months or more.
What role does the World Health Organization play during a flu pandemic?
The WHO coordinates global surveillance, issues strain recommendations for vaccines, and maintains the Pandemic Hub where countries share genomic sequences, case counts, and response strategies in real time.
Are masks still useful against influenza?
Yes. High‑filtration masks (N95/FFP2) reduce inhaled viral particles by up to 95%. Combined with ventilation and distancing, they form a strong barrier especially in crowded indoor settings.
What should I do if I’m exposed to the new H3N2 virus?
Take a rapid antigen test immediately, self‑isolate for 24‑48hours while awaiting results, and consider a short course of antiviral prophylaxis if you’re at high risk. Keep an eye on local health authority updates for guidance on isolation duration.





Gloria Reyes Najera
September 28, 2025 AT 12:25Look friends the US got the best labs and the fastest vaccine rollouts so we should lead the charge no one else can match our speed and resources we have the data pipelines and the tech to outpace any flu threat lets keep the momentum and show the world how it’s done
lee charlie
October 3, 2025 AT 03:51Hey everyone, it’s encouraging to see how quickly surveillance has caught the new H3N2 cases. The collaborative effort really shows what we can achieve together. Staying hopeful helps us keep pushing forward, and every piece of data makes a difference. Let’s keep supporting each other as we navigate this.
Greg DiMedio
October 7, 2025 AT 19:17Oh great, another flu pandemic and everyone pretends it’s a brand‑new crisis. Sure, we have mRNA now, but the basics stay the same – mask up, wash hands, and stop acting like it’s the end of the world. The hype machine loves a good scare, and the media will have us buying gadgets we don’t need.
Badal Patel
October 12, 2025 AT 10:42It is indeed prudent to reflect upon the annals of influenza pandemics, for history oft provides the most perspicacious counsel. The 1918 Spanish influenza, whilst catastrophic, suffered from an utter paucity of coordinated surveillance, thereby exacerbating mortality. In contrast, the 2009 H1N1 episode manifested the advantages of near‑real‑time data aggregation, a model which contemporary agencies have emulated. The present H3N2 emergence is distinguished by the expeditious deployment of genomic sequencing pipelines, allowing pathogen identification within a forty‑eight hour window. Such rapidity is a testament to the investments made in molecular diagnostics subsequent to the COVID‑19 epoch. Nevertheless, one must not be complacent; the production of egg‑based vaccines remains a bottleneck, often elongating lead times to several months. The advent of mRNA platforms promises to truncate this interval, yet scalability concerns persist due to raw material constraints. Moreover, public trust, a quintessential yet fragile asset, can be eroded by inconsistent messaging, as witnessed during the 1957 Asian flu. The current stratagem of transparent, multilingual briefings seeks to rectify this deficiency. Non‑pharmaceutical interventions, when applied in concert-masks, ventilation upgrades, and judicious school closures-have demonstrably attenuated transmission rates. Empirical models estimate a potential reduction of up to forty‑five percent when such measures are synergistically enforced. Additionally, the role of the World Health Organization’s Pandemic Hub cannot be overstated; it facilitates the rapid exchange of viral genomic data, thereby informing vaccine strain selection. Future preparedness should prioritize the establishment of decentralized vaccine manufacturing facilities, thereby mitigating reliance on centralized hubs. In parallel, investment in wastewater surveillance could furnish early community‑level alerts, complementing clinical testing regimes. Finally, the integration of artificial intelligence for outbreak prediction holds promise, yet its efficacy remains contingent upon the fidelity of input data. In sum, the amalgamation of robust surveillance, adaptable vaccine technologies, clear communication, and layered non‑pharmaceutical interventions constitutes the cornerstone of an effective pandemic response.
KIRAN nadarla
October 17, 2025 AT 02:08While the preceding exposition is undeniably thorough, one cannot overlook several linguistic imprecisions. The phrase "urgently" should have been employed rather than "urgent" in the context presented. Moreover, a comma is warranted after "In contrast," to preserve syntactic clarity. Nonetheless, the analytical depth is commendable, and the strategic recommendations merit serious consideration.
Kara Guilbert
October 21, 2025 AT 17:34We have a moral duty to protect the most vulnerable, and it’s disheartening to see anyone downplay the seriousness of this flu season. Ignoring the advice of experts is basically turning a blind eye to suffering, and that’s just not acceptable.
Sonia Michelle
October 26, 2025 AT 07:59When we examine the ebb and flow of pandemics, we see a pattern of collective responsibility intertwined with individual action. The choices we make-whether to vaccinate, to wear a mask, or to stay home when ill-resonate far beyond our personal spheres. It is a shared ethical contract that binds us together, especially in moments of crisis.
Neil Collette
October 30, 2025 AT 23:25Wow, look at that, the lofty philosopher tells us to wear a mask-next you’ll be preaching about flossing.
James Lee
November 4, 2025 AT 14:51Honestly, the whole “layered approach” is just a fancy way of saying we’re overcomplicating something simple: stay home when sick.
Dennis Scholing
November 9, 2025 AT 06:17Colleagues, let us consider a structured mentorship paradigm wherein experienced public‑health professionals guide community leaders on vaccine logistics, surveillance data interpretation, and risk communication. By fostering such mentorship, we empower local responders to act swiftly and effectively.
Kasey Lauren
November 13, 2025 AT 21:42That sounds great! I think everyone can learn a lot from seasoned pros, and it’ll help us feel more confident about the steps we take.
joshua Dangerfield
November 18, 2025 AT 13:08I'm curious about how wastewater surveillance data gets integrated into existing dashboards. Does anyone have a simple rundown of that process?
Abhimanyu Singh Rathore
November 23, 2025 AT 04:34Indeed, the integration is meticulous; one must first calibrate the qPCR thresholds, then map the spatial coordinates onto GIS layers, and finally employ statistical models to predict case surges-each step demanding rigorous validation. Moreover, adherence to standardized protocols ensures comparability across regions!
Stephen Lewis
November 27, 2025 AT 20:00Let us reaffirm our commitment to evidence‑based strategies, maintaining decorum and respect as we navigate these challenges together.
Lynn Kline
December 2, 2025 AT 11:25Well said-keep up the great work, team!