When you’re breastfeeding, every pill, injection, or drop you take doesn’t just affect you-it can reach your baby through your milk. That’s a real concern for thousands of new moms. You need your medication-for depression, infection, pain, or thyroid issues-but you also don’t want to risk your baby’s health. The good news? Medications in breast milk are rarely dangerous, and most are safe. The trick is knowing which ones are, and how they actually get there.
How Do Medications Even Get Into Breast Milk?
Breast milk isn’t just filtered blood. It’s made by special cells in your breasts that pull substances from your bloodstream. Most drugs cross into milk the same way water does: through passive diffusion. About 75% of medications move this way, flowing from areas of higher concentration (your blood) to lower concentration (your milk). It’s not magic-it’s physics. But not all drugs follow the same path. Some use special transporters, like tiny doors in the cell walls. Drugs like cimetidine and acyclovir hitch a ride on these, which is why they show up more in milk than you’d expect. Others, like heparin, are too big-over 800 daltons-and simply can’t squeeze through. That’s why blood thinners like heparin are considered safe: your baby gets almost nothing. Molecular size isn’t the only factor. Lipid solubility matters a lot. Drugs that dissolve easily in fat-like diazepam-cross more easily than water-soluble ones like gentamicin. That’s why a single dose of Valium can lead to noticeable drowsiness in a newborn, while an IV antibiotic like gentamicin barely registers in milk. Protein binding is another big player. If a drug is tightly stuck to proteins in your blood (like warfarin at 99%), it can’t float freely into milk. But sertraline? It’s 98.5% bound, yet still shows up in milk. Why? Because even 1.5% free drug is enough to cross, especially over time. And then there’s pH trapping. If a drug is a weak base (like amitriptyline), and your milk is slightly more acidic than your blood, the drug gets trapped in the milk, building up to 2-5 times higher levels than in your blood. That’s why some antidepressants need closer monitoring.Timing and Baby’s Age Make a Huge Difference
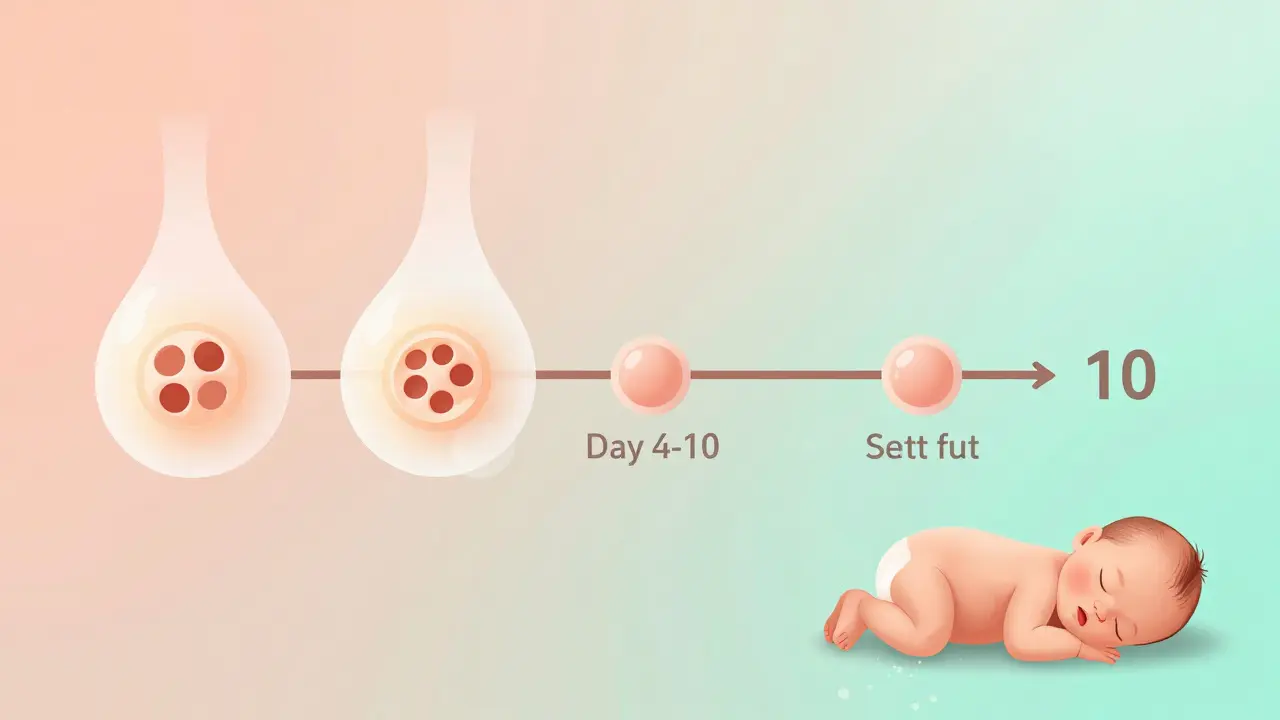
The first week after birth is the most critical. Your breast tissue is still changing. Between days 4 and 10, the tight connections between milk-producing cells aren’t fully closed yet. That means even larger molecules-like antibodies and some drugs-can slip through more easily. After day 10, those junctions seal up tight, and transfer drops by about 90%. Your baby’s age matters too. Newborns have underdeveloped livers and kidneys. They can’t clear drugs the way older babies or adults can. That’s why diazepam, with a half-life of 20-100 hours in adults, can stick around in a newborn for 30-100 hours. One dose can build up. That’s why doctors recommend avoiding long-acting benzodiazepines in early weeks unless absolutely necessary. Timing your doses helps. Taking your medication right after you breastfeed gives your body time to break down and clear the drug before the next feeding. Waiting 3-4 hours can cut your baby’s exposure by 30-50%. For drugs with short half-lives, like ibuprofen or amoxicillin, this simple trick makes a big difference.What Drugs Are Actually Safe?
Most medications you take are fine. The American Academy of Pediatrics says 87% of commonly prescribed drugs are “usually compatible” with breastfeeding. That includes:- Antibiotics: Amoxicillin, cephalexin, and azithromycin transfer minimally. Infant exposure is usually under 1-3% of the maternal dose.
- Pain relievers: Ibuprofen and acetaminophen are low-risk. They break down quickly and don’t accumulate.
- Antidepressants: Sertraline (Zoloft) is the go-to. Infant exposure is only 1-2% of the mom’s dose. Fluoxetine? Not as safe-it sticks around longer.
- Thyroid meds: Levothyroxine is safe. Your baby needs thyroid hormone, and this just replaces what you’re not making.
- Insulin and heparin: Too big to cross. Zero risk.
Which Drugs Should You Avoid-or Use With Caution?
Some drugs are riskier. The InfantRisk Center rates them from 1 (safe) to 5 (dangerous). Level 5 drugs, like radioactive iodine-131, require stopping breastfeeding completely. Level 4 includes lithium and certain chemotherapy drugs. But even here, context matters. For example, lithium: it crosses easily and can build up in babies, causing toxicity. But if you’re on a low dose and your baby’s levels are monitored weekly, many moms continue breastfeeding safely. The key is monitoring, not automatic quitting. Benzodiazepines like diazepam and clonazepam? Use sparingly. They can make babies sleepy, floppy, or cause feeding problems. If you need them, use the lowest dose for the shortest time. Avoid long-acting ones in the first month. High-dose estrogen birth control pills (over 50 mcg ethinyl estradiol) are a known milk supply killer. They can drop production by 40-60% in just 72 hours. Progesterone-only pills? Much safer. Many moms switch to them right after delivery.What About Antidepressants? The Biggest Concern for Moms
Depression during breastfeeding is common-and untreated, it’s more dangerous than most medications. But many moms stop breastfeeding because they’re scared of SSRIs. Sertraline is the best-studied. It’s the #1 prescribed antidepressant for breastfeeding moms. Studies show infant serum levels are typically below 10% of the mother’s therapeutic dose. Side effects? In 8.7% of cases, babies might be a little fussy. In 5.3%, they feed poorly. But these are mild and usually go away. Fluoxetine? Avoid in early weeks. It lasts too long in babies. Paroxetine? Also okay, but can cause more fussiness. Escitalopram? Good option, low transfer. The European Medicines Agency warns about serotonin syndrome-a rare but serious reaction. But the risk is extremely low. Only a handful of cases have been reported worldwide. The bigger risk? Stopping breastfeeding because you’re afraid.What About Nuclear Medicine or Imaging Tests?
A VQ scan? You’ll need to pump and dump for 12-24 hours. Tc-99m MAA transfers a little, and your baby gets a small radiation dose. But FDG-PET scans? You can breastfeed right after. Only 0.002% of the dose ends up in milk. No interruption needed. Mammograms? Safe. Contrast dye? Safe. MRI? Safe-even with gadolinium, since it doesn’t absorb well in the gut.
How Do You Know If It’s Safe for Your Baby?
Don’t guess. Use trusted resources. The InfantRisk Center’s LactMed app (version 3.2, updated January 2023) is the gold standard. It uses 12 pharmacokinetic factors to give you a real-time risk score. It’s free, updated monthly, and used by hospitals across the U.S. and Australia. Talk to your doctor, but also ask for a lactation consultant or pharmacist who specializes in breastfeeding. Most hospitals have them. They know the difference between “probably safe” and “safe with monitoring.”The Real Risk: Stopping Breastfeeding Unnecessarily
Here’s the truth: only 1-2% of medications absolutely require you to stop breastfeeding. Yet, 15-30% of moms quit because they’re told to-often without evidence. A 2022 study found that 56% of breastfeeding women take medication. Nearly 13% of them are on drugs that shouldn’t be used, not because they’re dangerous, but because no one told them how to use them safely. The CDC says medication concerns are the third most common reason moms stop breastfeeding-after low milk supply and nipple pain. That’s tragic. Most of those moms could have kept going. Your baby gets far more from your milk than you realize. Immune protection, better brain development, lower risk of obesity, asthma, and infections. And your mental health matters too. If you’re depressed, anxious, or overwhelmed, your baby feels it. A safe medication can help you be the mom you want to be.What to Do Next
If you’re on medication and breastfeeding:- Check the drug using LactMed or the InfantRisk Center website.
- Ask your doctor or pharmacist: “Is this safe for breastfeeding? What’s the infant exposure?”
- Time your doses: take right after a feed, wait 3-4 hours.
- Watch your baby: for sleepiness, fussiness, poor feeding, or unusual crying.
- Don’t stop without a plan. If you’re worried, get help-not advice from Google.
You don’t have to choose between being healthy and being a good mom. With the right info, you can do both.






Drew Pearlman
January 7, 2026 AT 13:31Wow, this is one of those posts that makes you realize how much science is actually working in your favor when you're breastfeeding. I didn’t know heparin couldn’t even cross into milk because it’s too big-that’s wild. I was so scared to take my blood thinner after my daughter was born, but now I feel way better about it. And the part about passive diffusion? It’s just physics, not some magical poison transfer. That alone calmed me down so much. I wish every OB had explained this in simple terms instead of just saying ‘ask your doctor’ and leaving you to Google it at 2 a.m. with a crying baby. Seriously, this should be mandatory reading for every new mom who’s on meds. The fact that 87% of meds are safe? That’s not a small number-that’s a lifeline. I’m sharing this with my mom’s group right now.
Also, timing doses after feeding? Genius. I started doing that with my ibuprofen and honestly, my baby’s been way less fussy. Small changes, huge impact. Thanks for writing this.
Also, LactMed? I just downloaded it. It’s like a secret weapon for breastfeeding moms who don’t want to guess.
And yes, stopping breastfeeding over fear is the real tragedy here. We’re not just feeding milk-we’re feeding trust, connection, safety. Don’t let misinformation take that away.
I’m so glad someone finally broke this down without fearmongering. You’re not a bad mom for needing meds. You’re a smart one for looking this up.
Also, thank you for mentioning that depression is more dangerous than SSRIs. I needed to hear that. I’ve been on sertraline for 8 months and my baby is thriving. We’re both okay.
Also, no, you don’t have to be perfect. You just have to be present. And meds help you be that.
Also, I cried reading this. Not because I was scared-but because I finally felt seen.
Also, if you’re reading this and you’re on meds and you’re scared? You’re not alone. We’re here. We’re doing it. And we’re doing it well.
Lindsey Wellmann
January 7, 2026 AT 20:40OMG I JUST FOUND OUT MY ANTIBIOTIC IS SAFE?? 😭💖 I’ve been pumping and dumping for 5 days because my nurse said ‘better safe than sorry’-but apparently I’ve been wasting 100 oz of gold liquid?? 🥲😭 I’m literally screaming right now. I just texted my husband: ‘HONEY WE CAN START BREASTFEEDING AGAIN.’ I’m going to cry again. I’m so mad I didn’t know this sooner. LactMed? I’m downloading it RIGHT NOW. Also, I’m going to send this to every mom in my WhatsApp group. We’ve all been terrified. We didn’t need to be. 😤💕 #BreastfeedingAndMedications #IJustGotMyLifeBack
Jerian Lewis
January 8, 2026 AT 12:06It’s irresponsible to say most meds are safe without emphasizing that ‘safe’ is a relative term. The data is observational, not controlled. Babies aren’t lab rats. You can’t just assume because a drug transfers in low amounts that it’s harmless over time. What about cumulative effects? What about the 1 in 1000 babies who are ultra-sensitive? You’re normalizing risk because it’s convenient. And you’re dismissing the mothers who’ve seen their babies become lethargic, irritable, or develop unexplained rashes after starting SSRIs. This post reads like a pharmaceutical brochure. Where’s the caution? Where’s the humility? We’re not talking about aspirin here-we’re talking about neuroactive compounds crossing into a developing brain. Don’t reduce this to a checklist. This is life.
Kiruthiga Udayakumar
January 9, 2026 AT 18:37As an Indian mom who breastfed for 2 years while on thyroid meds and antidepressants, I’m so tired of Western moms acting like this is new info. We’ve been doing this for decades. In India, most moms don’t have access to LactMed or pharmacists-they just ask their auntie or the local nurse. And guess what? Most of us are fine. My son is 8 now, brilliant, healthy, and he never knew I was on sertraline until I told him last year. He said, ‘Mom, you always smelled like love.’ That’s what matters. You don’t need an app to know if you’re doing right. You need your heart. And your gut. And your village. Stop over-medicalizing motherhood. We’ve been raising healthy babies with meds since before Google existed. 🙏❤️
tali murah
January 10, 2026 AT 12:02Oh, so now we’re supposed to believe that ‘1-2% of meds require stopping breastfeeding’? That’s a nice, clean statistic. But let’s not pretend the other 98% are benign. You gloss over the fact that infant exposure is measured in plasma levels, not in brain tissue. You don’t mention the long-term neurodevelopmental studies that show subtle differences in executive function in kids exposed to SSRIs in utero AND postnatally. And you completely ignore the fact that many of these ‘safe’ drugs are prescribed off-label to breastfeeding moms with zero pediatric safety data. This isn’t empowerment-it’s corporate reassurance dressed up as science. The fact that you recommend ‘timing doses’ like it’s a magic trick is laughable. Your baby’s liver doesn’t care when you took your pill. It only cares about what’s in the milk. And if you’re going to dismiss moms who worry as ‘fearful’ or ‘misinformed,’ then you’re part of the problem. This post is a beautifully written PR campaign. Not medical advice.
Diana Stoyanova
January 11, 2026 AT 06:23Let me just say this: motherhood is not a science experiment. It’s a sacred, messy, beautiful, terrifying dance between love and fear. And this post? It’s the kind of light that cuts through the fog. I was on fluoxetine for 6 months postpartum. My baby was fussy. I stopped. I spiraled. I thought I was failing. Then I found LactMed. I switched to sertraline. I waited 3 hours after feeding. I watched my baby like a hawk. And guess what? He smiled at 8 weeks. He slept through the night at 12. He’s 3 now and runs like a cheetah. I didn’t choose between being a mom and being well-I chose to be both. And you can too. Don’t let fear steal your joy. Don’t let silence steal your strength. You are not alone. You are not broken. You are not failing. You are showing up. And that? That’s enough. And if you need meds to show up? Then take them. With pride. With courage. With your head held high. Because you’re not just feeding milk. You’re feeding hope. And that? That’s the most powerful medicine of all. 💪🍼❤️
Elisha Muwanga
January 11, 2026 AT 13:50Let’s be real-this whole ‘breastfeeding is best’ narrative is just a marketing ploy by Big Pharma and the lactation industrial complex. You’re scaring moms into feeling guilty for not breastfeeding while simultaneously pushing them to take drugs that could harm their babies. And you act like it’s a choice? It’s not. It’s coercion wrapped in virtue signaling. Who decided milk is the only way to bond? Formula-fed kids grow up fine. In fact, they’re often healthier because they’re not getting random pharmaceutical residues. And don’t get me started on the ‘depression is worse than SSRIs’ line. That’s a cop-out. Why not fix the system? Why not give moms paid leave, childcare, therapy, and real support instead of telling them to swallow pills and keep pumping? This post is a distraction. The real problem isn’t medication in breast milk-it’s that we don’t support mothers at all.
Maggie Noe
January 12, 2026 AT 18:38Jerian and Tali-I hear you. The science isn’t perfect. The data is limited. And yes, we’re asking moms to make decisions with incomplete information. But here’s the thing: we’re not asking them to guess. We’re asking them to *inquire*. To use tools. To talk to specialists. To weigh risk vs. benefit. And yes, some moms will have bad outcomes. But the majority? They’ll thrive. And the ones who don’t? We owe them better research-not silence. This isn’t about pushing meds. It’s about removing shame. I’ve been a NICU nurse for 15 years. I’ve seen babies born to moms on every kind of drug. Some had issues. Most didn’t. And the ones who struggled? It wasn’t the sertraline. It was the isolation. The lack of support. The fear. The guilt. That’s what breaks mothers. Not the pill. So yes, use LactMed. Time your doses. Watch your baby. But please-don’t let the perfect be the enemy of the good. We’re not trying to make motherhood risk-free. We’re trying to make it possible. And sometimes, that means taking a pill and still holding your baby close. And that’s brave. Not reckless. Not irresponsible. Brave.