Tendering Process in Pharmacy: How Medications Are Selected and Purchased
When you pick up a prescription at the pharmacy, you rarely think about how that drug got there. But behind every pill, injection, or capsule is a complex tendering process, a formal system used by hospitals, governments, and insurers to select and purchase medications at the best price while ensuring safety and availability. Also known as pharmaceutical procurement, this system determines which generic versions of drugs like rosuvastatin or azithromycin end up on shelves, and which brand-name options get approved for coverage. It’s not just about cost—it’s about trust, regulation, and real-world outcomes.
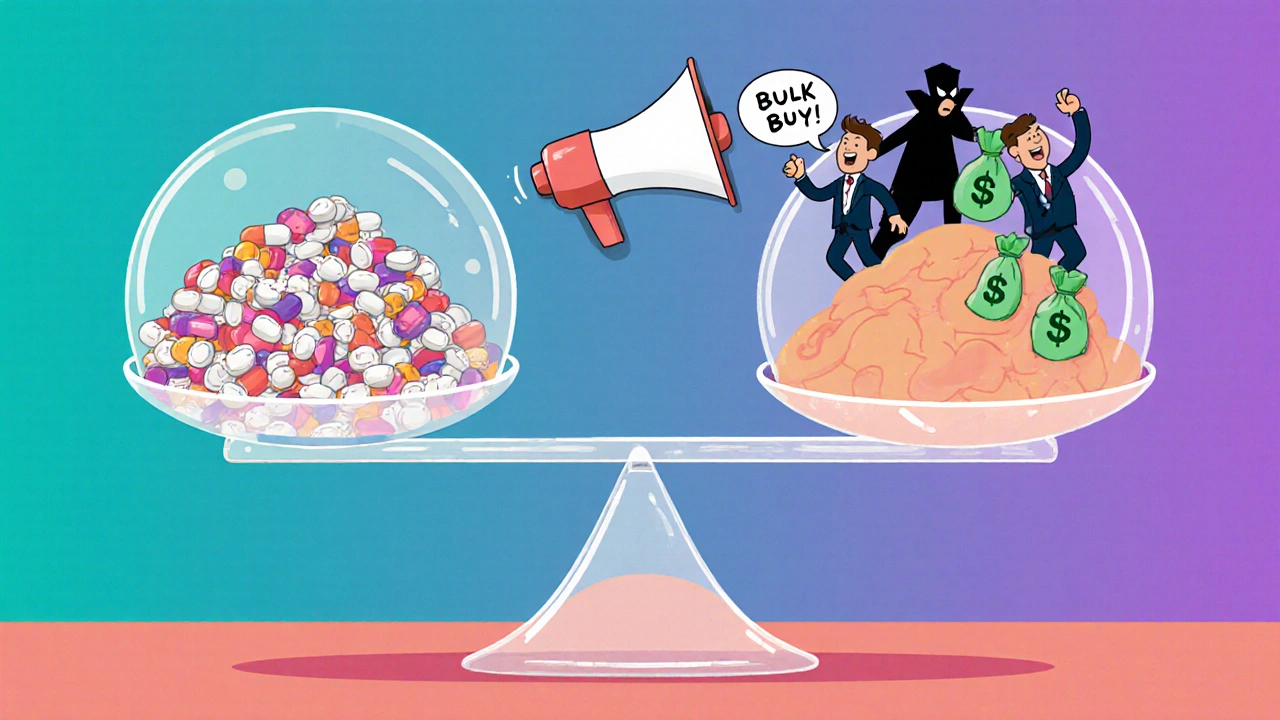
This process isn’t random. Public health systems, insurance providers, and large hospital networks run competitive bids where manufacturers submit proposals to supply drugs at fixed prices. The lowest bid doesn’t always win. Agencies check for FDA compliance, past performance, batch consistency, and even post-market safety data. For example, the FDA’s Post-market surveillance, the ongoing monitoring of drugs after they’re approved. Also known as FDA Sentinel Initiative, it helps identify if a generic version has hidden risks like QT prolongation or unexpected side effects. If a batch of generic Crestor shows higher rates of muscle pain in real patients, that manufacturer could be disqualified from future bids. The tendering process doesn’t just pick the cheapest drug—it picks the safest one that still saves money.
And it’s not just about big systems. Even small clinics and community pharmacies use simplified versions of this process when they negotiate with wholesalers. They look at lead times, return policies, and whether the supplier provides accurate labeling—something you can verify yourself by checking your medication label, the printed information on your prescription bottle that should include the prescriber’s name, pharmacy details, and correct drug strength. Also known as prescription safety, this step protects you from dangerous mix-ups. If a pharmacy gets a bad batch through a shady supplier, you’re the one who might end up with the wrong dose or inactive ingredient. That’s why transparency in the tendering process matters to everyone, not just administrators.
What you’ll find in the posts below are real stories from people who’ve been affected by these decisions. From how switching from brand to generic can trigger side effects, to why some drugs like vardenafil or azathioprine are chosen over others based on procurement rules, to how parents in pediatric care fight to get the right blood thinners for their kids—every post ties back to how these behind-the-scenes deals shape your health outcomes. You won’t just learn how the system works. You’ll learn how to spot when it’s working for you—and when it’s not.