Probiotic Dosage Calculator
Help Reduce Antibiotic Side Effects
This calculator helps determine the appropriate probiotic strain, dosage, and timing based on your antibiotic treatment to reduce the risk of antibiotic-associated diarrhea (AAD) and C. diff.
Input Your Antibiotic Treatment
Your Probiotic Recommendation
Recommended Strain
Most EffectiveLactobacillus rhamnosus GG (Most studied for antibiotic use)
Dosage
Daily10 billion CFUs per day
Timing Instructions
Critical
Take probiotics 2-3 hours after your antibiotic dose
Start on same day as antibiotics
Continue for 1-2 weeks after finishing antibiotics
Important Contraindications
Do NOT take probiotics if:
- Immunocompromised (cancer treatment, HIV, organ transplant)
- Have a central IV line
- Recently had major surgery
- Have severe pancreatitis
- Have a known yeast allergy (if taking S. boulardii)
When you’re on antibiotics, you might expect to feel better - but instead, you get bloating, cramps, or worse, watery diarrhea. It’s not just bad luck. Antibiotics don’t just kill the bad bacteria; they wipe out the good ones too. Your gut, home to over 100 trillion bacteria, gets thrown out of balance. That’s where probiotics come in. They’re not magic pills, but for many people, they help prevent or lessen the gut chaos that comes with antibiotics.
Why Antibiotics Mess With Your Gut
Antibiotics are powerful. They target bacteria causing infections - but they don’t pick and choose. They hit everything. That includes the helpful microbes in your intestines that help digest food, make vitamins, and keep your immune system sharp. When these good bacteria drop, harmful ones like Clostridioides difficile (C. diff) can take over. C. diff causes severe diarrhea and can lead to hospitalization. About 5% to 30% of people on antibiotics get some form of antibiotic-associated diarrhea (AAD). For hospitalized patients, that number jumps higher.What Do Probiotics Actually Do?
Probiotics are live bacteria and yeasts that are meant to restore balance. Think of them as reinforcements for your gut. The most studied strains for antibiotic use are Lactobacillus rhamnosus GG, Saccharomyces boulardii, and certain Bifidobacterium species. These don’t just fill space - they compete with harmful bugs, strengthen the gut lining, and produce substances that calm inflammation. A major Cochrane review in 2020 looked at 2,454 people across 13 studies. Those who took probiotics while on antibiotics had just a 3.1% chance of developing C. diff diarrhea. The group that didn’t take probiotics? 11.6%. That’s a 73% drop in risk. For general antibiotic diarrhea, the benefit was still clear: probiotics cut the odds by nearly half in many cases. Saccharomyces boulardii, a yeast probiotic, showed up in studies as reducing AAD risk by 50%.Not All Probiotics Are Created Equal
Here’s the catch: not every probiotic works for every problem. A product labeled “probiotic” could contain anything - and often doesn’t contain what it claims. A 2022 ConsumerLab test found that 30% of probiotic supplements didn’t have the number of live organisms listed on the label. Fifteen percent even had extra, unlisted microbes. For antibiotic-related issues, stick to strains with real evidence:- Lactobacillus rhamnosus GG - Most studied, widely available in brands like Culturelle. Proven to reduce diarrhea.
- Saccharomyces boulardii - A yeast, not a bacteria. Works even when taken with antibiotics. Reduces risk by about half.
- Bifidobacterium lactis and Bifidobacterium longum - Often found in multi-strain blends. Helpful for bloating and gas.
When and How to Take Them
Timing matters. Antibiotics can kill probiotics if they’re taken at the same time. Most experts recommend spacing them out by 2 to 3 hours. Take your antibiotic, then wait a few hours before your probiotic. Some people take the probiotic at bedtime, when the antibiotic has cleared their system. Take probiotics daily - not just when symptoms start. Start on the same day as your antibiotic and keep going for at least one to two weeks after you finish the course. This gives your gut time to rebuild. Some probiotics work better on an empty stomach; others need food to survive stomach acid. Check the label. Acid-resistant strains like L. rhamnosus GG can be taken without food. If you’re unsure, take it with a light meal.
Side Effects - And When to Worry
Most people feel fine. But in the first few days, you might notice more gas, bloating, or even constipation. That’s normal. Your gut is adjusting. These usually fade within a week. But there are red flags. If you’re immunocompromised - due to cancer treatment, HIV, organ transplant, or severe autoimmune disease - probiotics can be dangerous. There have been rare cases of bloodstream infections from Lactobacillus and Saccharomyces boulardii. People with central lines, recent surgery, or who are critically ill should avoid them unless a doctor says it’s safe. If you have IBS or a sensitive gut, probiotics might make things worse at first. Start with a lower dose - maybe 1-2 billion CFUs - and see how you feel before increasing.What the Research Really Says
Yes, probiotics help. But the science isn’t perfect. Some studies show big benefits. Others show almost none. Why? Because probiotics aren’t one-size-fits-all. A strain that works for amoxicillin might not help with ciprofloxacin. And some research suggests certain probiotics might even slow down your gut’s natural recovery after antibiotics. The 2020 Cochrane review rated the evidence as “moderate” - not high. That means we’re confident enough to recommend them for most people, but we’re still learning. The NIH is now funding $12.5 million in new studies to figure out which strains work best for which antibiotics and patient groups.Regulation? There Isn’t Much
In the U.S., probiotics are sold as dietary supplements. That means manufacturers don’t have to prove they work or are safe before selling them. The FDA doesn’t test them. Labels can be misleading. A bottle might say “10 billion CFUs,” but if the product isn’t stored right - or if it’s old - those numbers could be way lower. That’s why buying from trusted brands matters. Look for ones that list exact strains, CFU counts, and expiration dates. Brands that use third-party testing (like USP or ConsumerLab) are more reliable. Don’t just pick the cheapest one on the shelf.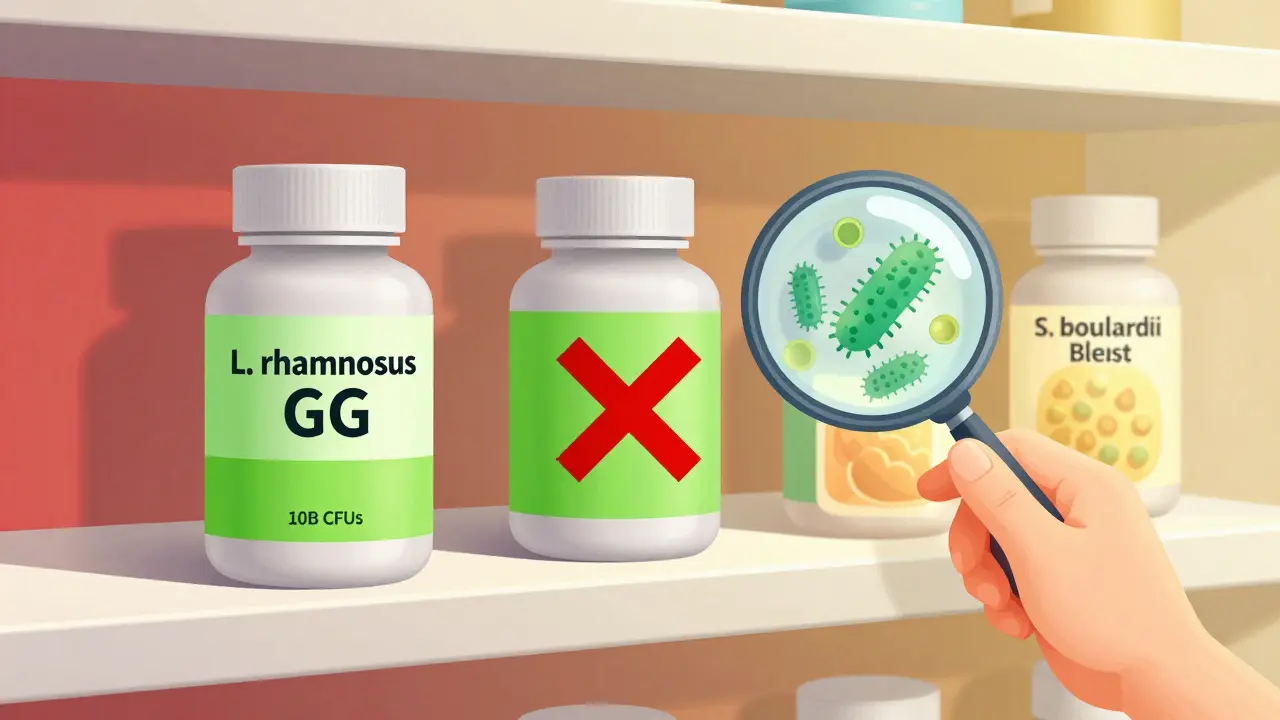
Real People, Real Results
On Amazon, Culturelle (L. rhamnosus GG) has over 12,500 reviews with a 4.2-star rating. Many users write: “No diarrhea this time,” or “My stomach stayed calm while on antibiotics.” But there are also 15% of negative reviews that say, “Nothing changed.” And 10% say, “It made me worse.” That’s the reality. It works for many, not all. Reddit communities like r/Probiotics are full of people sharing their timing tricks - taking probiotics at night, switching brands, combining with prebiotic fiber. These aren’t clinical trials, but they show what works in daily life.Who Should Skip Probiotics?
You should avoid probiotics if you:- Have a weakened immune system
- Are critically ill or in the ICU
- Have a central IV line or recent major surgery
- Have a known allergy to yeast (if taking S. boulardii)
- Have severe pancreatitis
What to Do Next
If you’re about to start antibiotics:- Ask your doctor if probiotics are right for you.
- Choose a product with L. rhamnosus GG or S. boulardii.
- Make sure it has at least 5-10 billion CFUs per dose.
- Take it 2-3 hours after your antibiotic.
- Keep taking it for 1-2 weeks after your antibiotics end.
What’s Next for Probiotics?
The future isn’t about generic probiotics. It’s about precision. Researchers are starting to match specific strains to specific antibiotics and patient profiles. Imagine a probiotic prescription tailored to your drug, your age, your gut health. That’s coming - but it’s not here yet. For now, the best advice is simple: use proven strains, take them correctly, and don’t expect miracles. Probiotics won’t fix everything - but for many, they make the difference between a rough week and a manageable one.Can I get probiotics from yogurt instead of supplements?
Yes, but it’s not ideal. Yogurt contains live cultures, but the strains and amounts vary widely. Most commercial yogurts have far fewer CFUs than what’s used in studies (often less than 1 billion). Plus, many have added sugar, which can worsen gut issues. For reliable results during antibiotic therapy, supplements with clearly labeled strains and doses are better.
How long should I take probiotics after finishing antibiotics?
Continue for at least one to two weeks after your last antibiotic dose. Your gut needs time to rebuild its balance. Stopping too soon might let harmful bacteria bounce back. Some people choose to keep taking them longer - especially if they still feel bloated or irregular - but there’s no harm in doing so, as long as you’re not experiencing side effects.
Do probiotics interfere with antibiotics?
No, they don’t interfere with how antibiotics kill bacteria. But if you take them at the same time, the antibiotic can kill the probiotic bacteria before they reach your gut. That’s why spacing them 2-3 hours apart is important. Probiotics work best when they’re not being wiped out right away.
Are there any foods I should avoid while taking probiotics?
Not really. But avoid excessive sugar and highly processed foods - they feed bad bacteria and can undo some of the benefits. Focus on fiber-rich foods like vegetables, legumes, and whole grains. These act as prebiotics, helping good bacteria grow. Alcohol and artificial sweeteners may also irritate your gut, so limit them while on antibiotics and probiotics.
Can kids take probiotics with antibiotics?
Yes, and they often benefit even more than adults. Studies show probiotics reduce diarrhea in children on antibiotics by about 50%. Use age-appropriate doses - typically 5-10 billion CFUs for kids. L. rhamnosus GG is the most studied for children. Always check with your pediatrician first, especially if your child has a compromised immune system.






John Brown
December 16, 2025 AT 15:33Been on antibiotics twice this year and switched to Culturelle after the first time I got wrecked by diarrhea. Second time? Zero issues. Just take it 3 hours after your pill, bedtime works great. Seriously, it’s not magic but it’s the closest thing.
John Samuel
December 17, 2025 AT 03:21One must acknowledge the profound epistemological implications of microbiome modulation in the context of antimicrobial stewardship. The probiotic paradigm, particularly with Saccharomyces boulardii, represents a paradigmatic shift in gastroenterological prophylaxis - a veritable triumph of translational science over empirical neglect. 🧬🔬
Benjamin Glover
December 18, 2025 AT 03:20Probiotics? Please. Americans think yogurt is medicine. In the UK, we just eat soup and get on with it.
Michelle M
December 19, 2025 AT 19:42I used to think probiotics were just hype until I started taking them with my antibiotics. I didn’t just avoid diarrhea - I felt calmer. Like my gut was finally getting a break from the chaos. Maybe it’s not just bacteria. Maybe it’s peace.
Cassie Henriques
December 21, 2025 AT 10:32CFU titration is critical - most OTC products lack strain-specific validation and are subject to significant viability decay under non-refrigerated storage. The 2022 ConsumerLab meta-analysis revealed alarming heterogeneity in label accuracy, particularly with Lactobacillus spp. in ambient-temperature formulations. Always verify third-party certification.
Jake Sinatra
December 23, 2025 AT 02:31As a medical professional, I recommend probiotics to every patient on antibiotics - but only if they use evidence-based strains, proper dosing, and correct timing. Don’t gamble with your gut health. This isn’t a supplement. It’s preventive medicine.
RONALD Randolph
December 23, 2025 AT 21:22Probiotics? That’s just a scam! The FDA doesn’t regulate them - so of course they’re full of crap! You think some guy in a warehouse in China can just toss some bacteria into a capsule and call it science? NO! NO! NO! You’re just feeding your gut junk!
Raj Kumar
December 25, 2025 AT 15:31in india we use curd with a pinch of salt after antibiotics. not fancy but works. my uncle took 10 days of abx and just ate curd daily - no issues. probiotic pills? too expensive for most here.
Melissa Taylor
December 27, 2025 AT 03:53I started taking probiotics after my last round of antibiotics and honestly, I didn’t notice much. But I kept going anyway. Better safe than sorry, right? And I like knowing I’m doing something good for my body.
Christina Bischof
December 28, 2025 AT 01:22took mine at night and didn’t think about it again. no drama. no magic. just… didn’t get sick. that’s good enough for me.
Jocelyn Lachapelle
December 28, 2025 AT 17:16My grandma used to say, ‘Your gut is your second brain.’ She never heard of probiotics, but she ate fermented things every day. Turns out she was onto something. Sometimes the old ways are just the first science.