When a drug safety alert pops up-whether it’s a recall notice, a warning about side effects, or a change in dosage guidelines-it’s easy to feel like the ground just dropped out from under you. Your heart races. Your breath gets shallow. Your mind spins through worst-case scenarios. You might feel like you need to act immediately, even if you don’t fully understand what’s happening. This isn’t just stress. It’s a biological survival response kicking in, and it’s designed to shut down clear thinking. The good news? You don’t have to let it control your decisions.
Why Alerts Trigger Panic (And Why It’s Not Your Fault)
Your brain doesn’t distinguish between a tiger in the bushes and a drug safety alert on your phone. When your nervous system detects a threat-even a digital one-it flips into fight-or-flight mode. Blood rushes to your muscles. Your heart rate spikes to 110-130 beats per minute. Your prefrontal cortex, the part of your brain responsible for logic and planning, gets sidelined. In this state, you’re not thinking. You’re reacting. Studies show that during panic, people lose up to 67% of their ability to weigh options carefully. That’s why so many people end up stopping a medication cold turkey, calling their doctor in a frenzy, or googling symptoms until they convince themselves they’re having a rare reaction. None of those actions are wrong by nature-but when they’re driven by panic, they’re often counterproductive.Step 1: Pause Before You Act
The first rule of responding to any alert? Don’t respond immediately. Give yourself 90 seconds. That’s all it takes to begin calming your nervous system. Start with your breath. Inhale slowly through your nose for four counts. Hold for seven. Exhale through your mouth for eight. Repeat three times. This isn’t just a relaxation trick. It’s a neurological reset. Research from Pacific Coast Mental Health shows this 4-7-8 breathing technique lowers heart rate from panic levels to 70-85 bpm in under two minutes-enough to bring your thinking brain back online. If you’re in a high-stress environment-like a pharmacy, hospital, or even your home with kids around-try the TIPP method: Temperature, Intense exercise, Paced breathing, and Paired muscle relaxation. Splash cold water on your face. Do 30 seconds of jumping jacks. Tighten your fists for five seconds, then release. These aren’t gimmicks. They’re science-backed tools used by emergency responders and trauma therapists to break the panic cycle.Step 2: Ground Yourself in Reality
Panic pulls you into the future-imagining disasters that haven’t happened. Grounding brings you back to the present. Try the 5-4-3-2-1 technique. Look around and name:- 5 things you can see
- 4 things you can touch
- 3 things you can hear
- 2 things you can smell
- 1 thing you can taste
Step 3: Separate the Alert from the Assumption
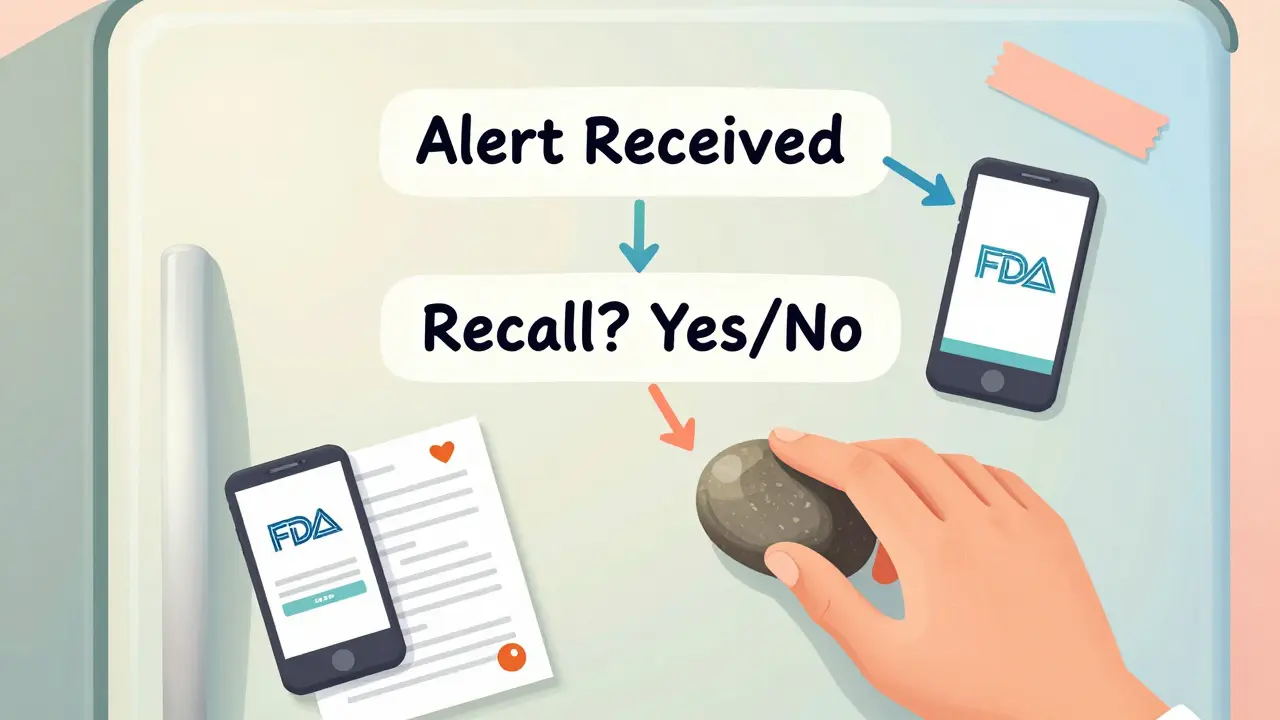
Drug safety alerts are often written in alarming language. Words like “serious,” “risk,” “warning,” and “discontinue” are designed to get attention. But they don’t always mean what you think they mean. A warning about “increased risk of dizziness” doesn’t mean you’ll collapse. It means a small percentage of users reported mild lightheadedness in clinical trials. Ask yourself: What exactly is the alert saying? What’s the source? Is it from the FDA, the TGA (Therapeutic Goods Administration), or a private research group? Is it based on a single case report or a large study? Write it down. Don’t rely on memory. Write the exact wording of the alert, the date it was issued, and the agency behind it. This simple act of documentation reduces ambiguity-and with it, fear.Step 4: Use a Decision Flowchart
When your brain is overwhelmed, complexity kills. Create a simple flowchart for yourself ahead of time. Print it. Tape it to your fridge. Save it on your phone. Here’s a basic version:- Is this a recall? (Official government notice) → Stop medication immediately. Contact pharmacy.
- Is this a warning? (Potential side effect) → Don’t stop. Note symptoms. Schedule doctor appointment.
- Is this a dosage change? → Check updated prescribing guide. Call pharmacist to confirm.
- Is this a rumor or social media post? → Ignore. Verify with official source.
Step 5: Align Decisions with Your Values
Ask: “What matters most to me right now?” Is it safety? Stability? Avoiding hospital visits? Minimizing side effects? Your answer guides your next move. If your core value is avoiding unnecessary disruption, you might choose to monitor symptoms and schedule a check-up instead of stopping the drug. If your value is minimizing risk at all costs, you might contact your prescriber for an alternative. Neither is right or wrong. But when your decision comes from your values-not your fear-you’ll feel more confident, even if the outcome isn’t perfect.Prepare Before the Alert Happens
Most people fail at managing panic not because they’re weak, but because they never practiced. Just like you wouldn’t wait until a fire to check your smoke alarm, don’t wait until a drug alert to learn how to respond. Build a personal alert response kit:- A printed copy of your current medications and dosages
- A list of your pharmacy’s phone number and your doctor’s contact info
- A small object for tactile grounding-a smooth stone, a keychain, a mint
- A printed version of your decision flowchart
- A journal entry template: “Trigger: ___. My reaction: ___. What I did: ___. Outcome: ___.”
What to Do When You’re Still Unsure
If you’re still stuck after trying these steps, call your pharmacist. They’re trained to interpret alerts and can explain what it means for your specific situation. Don’t wait for your doctor if they’re not available-pharmacists are often the first line of defense in drug safety. Avoid these common mistakes:- Stopping medication without professional advice (unless it’s a recall)
- Searching symptoms online (Google doesn’t know your medical history)
- Waiting too long to act (if you feel severely unwell, seek help)
- Blaming yourself for feeling panicked (it’s biology, not weakness)
Industry Trends Show This Is No Longer Optional
This isn’t just about personal calm. It’s becoming a standard in healthcare. Starting in January 2025, the European Union’s DORA regulation requires all digital health systems to include human behavior considerations in alert design. Hospitals in the U.S. and Australia are now training staff in panic response techniques. The TGA has begun recommending that prescribers provide patients with simple alert response guides. Even tech companies are catching on. New wearable devices can detect when your heart rate spikes after an alert and automatically trigger a calming breathing exercise on your phone. AI-powered alert systems are being tested to guide users through questions like: “Have you taken your medication today?” or “Are you experiencing new symptoms?”-reducing panic-driven reactions by over 50% in trials.You’re Not Alone
78.6% of people who experience panic during health alerts respond positively to structured techniques when practiced regularly. You’re not broken. You’re human. And with the right tools, you can turn panic into clarity. The goal isn’t to never feel afraid. It’s to never let fear make your decisions for you.What should I do first when I get a drug safety alert?
Stop, breathe, and pause for 90 seconds. Use the 4-7-8 breathing technique: inhale for 4 seconds, hold for 7, exhale for 8. This calms your nervous system enough to think clearly. Don’t act until your heart rate drops and your thoughts stop racing.
Should I stop taking my medication right away?
Only if it’s an official recall from the TGA, FDA, or another government agency. Most alerts are warnings, not stop orders. Stopping medication abruptly can be dangerous-especially for antidepressants, blood pressure drugs, or seizure medications. Always verify the alert’s source and consult your pharmacist before making changes.
How do I know if an alert is real or just fear-mongering?
Check the source. Official alerts come from government health agencies like the TGA (Australia), FDA (U.S.), or EMA (Europe). Avoid social media posts, blogs, or unsolicited emails. Look for the issuing agency’s logo, a date, and a reference number. If you’re unsure, call your pharmacy-they can verify it in seconds.
Can I use these techniques for other types of alerts, like cybersecurity or emergency warnings?
Yes. These techniques work for any high-stress alert-whether it’s about your medication, your bank account, or a weather emergency. Panic response is universal. The 5-4-3-2-1 method, controlled breathing, and grounding objects help you stay calm no matter the trigger.
Why do I still feel anxious even after following the steps?
It’s normal. Anxiety doesn’t vanish instantly. The goal isn’t to feel zero fear-it’s to act despite it. If you still feel uneasy, write down your concerns and schedule a follow-up with your doctor or pharmacist. Sometimes, anxiety lingers because there’s still uncertainty. A professional conversation can resolve that.






Akshaya Gandra _ Student - EastCaryMS
January 4, 2026 AT 18:26Dee Humprey
January 6, 2026 AT 15:28Jacob Milano
January 7, 2026 AT 21:55en Max
January 8, 2026 AT 10:46melissa cucic
January 8, 2026 AT 21:12Angie Rehe
January 9, 2026 AT 15:52Aaron Mercado
January 11, 2026 AT 02:56Enrique González
January 11, 2026 AT 08:34