Bone Marrow Disorders: Causes, Types, and Treatments
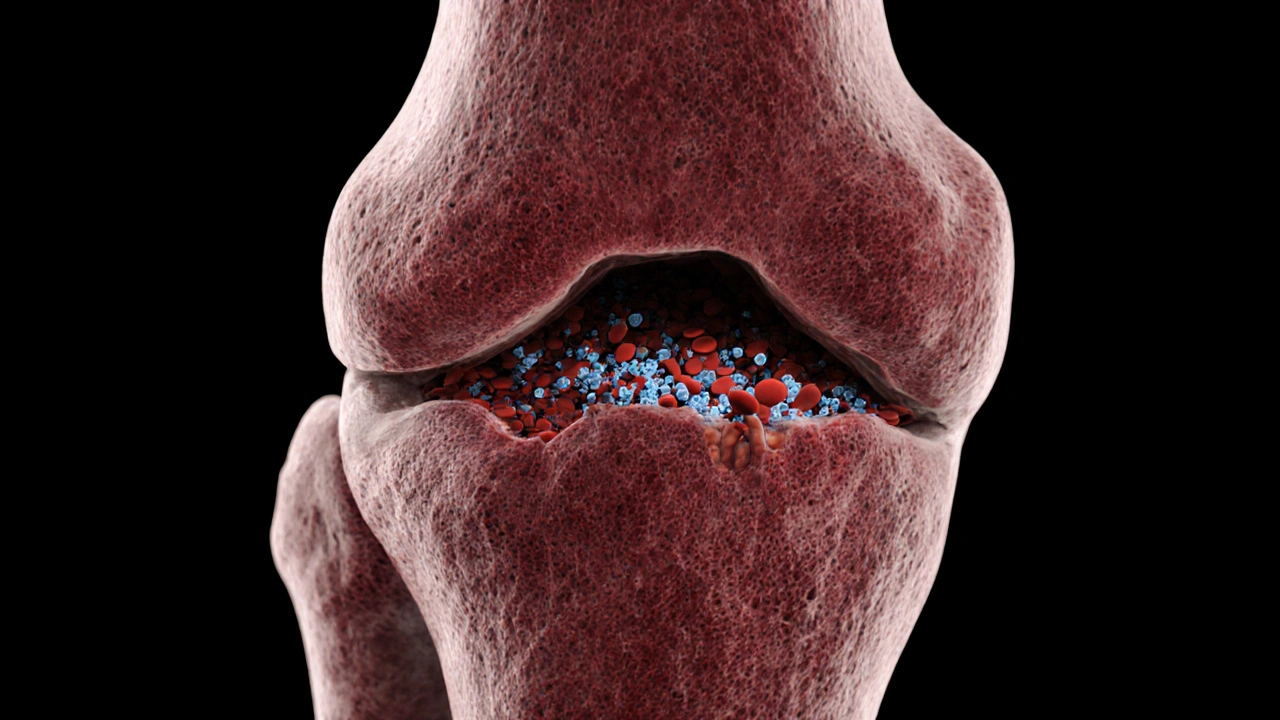
When exploring bone marrow disorders, a group of conditions that disturb the marrow’s ability to produce healthy blood cells, it’s useful to map the landscape first. These disorders bone marrow disorders range from malignant cancers to benign failures, and each brings its own set of challenges for patients and doctors.
One of the biggest sub‑categories is Leukemia, a cancer of white blood cells that typically originates in the marrow. Another common condition is Aplastic anemia, a rare but serious failure of the marrow to produce enough new blood cells. Then there are Myelodysplastic syndromes, a collection of disorders where the marrow makes abnormal blood cells that don’t function properly. All of these entities share a core problem: the marrow can’t keep up with the body’s demand for red cells, white cells, and platelets. Because of that, treatment often leans on bone marrow transplant, a procedure that replaces damaged marrow with healthy donor cells to reset blood production.
Key Types and Their Impact
Understanding how each disorder works helps you see why symptoms overlap yet differ in severity. Leukemia usually shows up with persistent fatigue, easy bruising, and frequent infections because cancerous white cells crowd out normal ones. Aplastic anemia presents similarly—fatigue, shortness of breath, and bleeding—but the underlying cause is immune‑mediated destruction of stem cells, not cancer. Myelodysplastic syndromes often start with mild anemia and evolve slowly, sometimes progressing to acute leukemia if left unchecked. Recognizing these patterns early can prompt a timely bone marrow biopsy, which remains the gold‑standard diagnostic tool across all four conditions.
Once a diagnosis is confirmed, the next step is figuring out the right treatment path. For many patients with aggressive leukemia, chemotherapy followed by a bone marrow transplant offers the best chance of remission. In contrast, mild aplastic anemia may respond to immunosuppressive drugs alone, while more severe cases still need a transplant. Myelodysplastic syndromes have a spectrum of treatment options—from supportive care with blood transfusions to hypomethylating agents and, when appropriate, transplant. The common thread is that each approach aims to restore the marrow’s ability to churn out functional cells.
Beyond medical therapy, lifestyle adjustments play a quiet yet vital role. Maintaining adequate iron and folate intake supports red‑cell production, while avoiding infections through good hygiene reduces complications for immunocompromised patients. Regular monitoring of blood counts lets doctors catch trouble early, whether it’s a rising blast count in leukemia or a sudden drop in platelets in aplastic anemia. This proactive stance can mean the difference between an elective transplant and an emergency procedure.
Below you’ll find a curated collection of articles that dive deeper into each of these topics. From practical tips on managing chemotherapy side effects to step‑by‑step guides on finding a compatible donor, the posts are organized to give you quick, actionable insight. Explore the list to learn more about the disorders, their diagnoses, and the latest treatment strategies tailored to each condition.