Bronchial Asthma is a chronic respiratory disease where the airways become inflamed and overly sensitive, causing wheeze, cough and breathlessness. When you add a plane ticket or a road‑trip itinerary into the mix, the challenge shifts from daily symptom control to staying safe on the move. Below are actionable tips that let you enjoy the journey without compromising your lungs.
Quick Takeaways
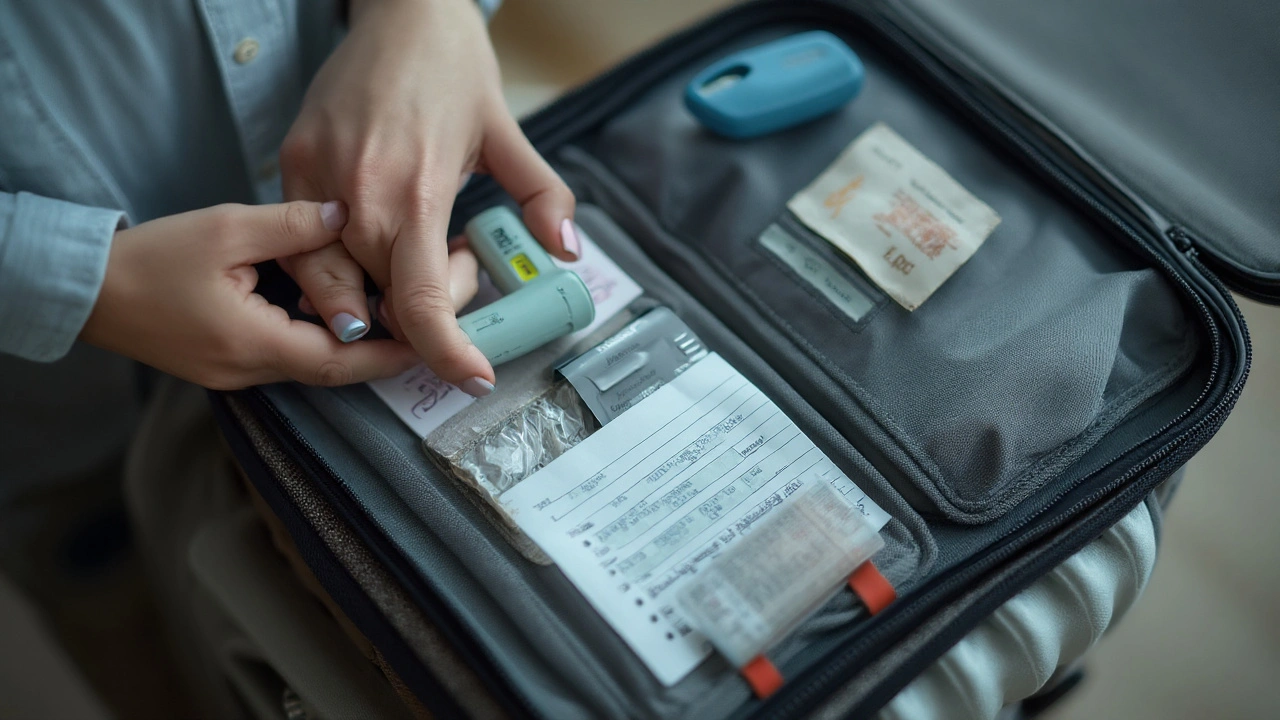
- Carry a rescue Inhaler (quick‑relief device) in your hand‑luggage.
- Check the Air Quality Index (AQI) forecast for your destination.
- Bring a portable Peak Flow Meter to monitor lung function each day.
- Write an Emergency Action Plan that lists meds, contacts and steps and share it with travel companions.
- Consider Travel Insurance covering asthma‑related emergencies.
Understanding the Core Triggers
While bronchial asthma travel may sound daunting, knowing the main environmental culprits makes prevention easier. Common triggers include sudden changes in Altitude (lower oxygen pressure at higher elevations), temperature extremes, pollen spikes, and poor indoor air quality inside cabins or hotels. Each of these factors can tighten airways, so a proactive plan is essential.
Pre‑Travel Medical Prep
Start the checklist at least two weeks before departure. Schedule a review with your Respiratory Specialist who can adjust medication dosages for travel stress. Request a written prescription for your rescue inhaler and any controller drugs, and ask for a doctor’s letter that explains the necessity of carrying them through security.
Ask about a COVID‑19 or influenza vaccination if you haven’t had one recently; infections are a leading cause of asthma exacerbations abroad. Pack a 30‑day supply of all meds, plus a spare set in a separate bag in case luggage is delayed.
Managing Triggers on the Move
When you board a plane, the cabin air is recirculated and often dry, which can irritate the airways. Keep a small bottle of saline spray handy and use it before and after the flight. If you’re traveling by car, keep windows slightly open or use the AC’s “fresh air” setting to avoid stagnant buildup of pollen or exhaust fumes.
Smartphones can be lifesavers: download an AQI app that gives real‑time readings for the city you’re visiting. Pair it with a weather app that highlights humidity levels-high humidity can worsen mucus production, while very dry air may trigger bronchoconstriction.
In‑Flight Strategies
Carry your inhaler in a clear plastic pouch to speed up security checks. If you need a spacer (a device that improves medication delivery), pack it disassembled to meet airline regulations; many airlines allow medical devices that are declared at the gate.
During the flight, take a deep breath and use your inhaler if you feel tightness, even if symptoms seem mild. The lower oxygen pressure at cruising altitude can mask early warning signs, so a pre‑emptive puff often prevents a full‑blown attack.

Destination Considerations
Research the local climate before you land. High‑altitude cities like La Paz or Denver require a gradual acclimatization period; consider staying at a lower elevation for the first 24‑48hours. For tropical destinations with high pollen counts (e.g., parts of Australia, Southeast Asia), schedule outdoor activities in the early morning when pollen levels are lowest.
Hotel rooms with air‑conditioning that includes HEPA filtration provide the cleanest indoor air. If you’re staying in a budget hostel, bring a portable air‑purifier or a small fan to keep dust from settling.
Emergency Planning
An Emergency Action Plan is a written set of steps for managing a sudden asthma flare‑up should be sealed in a waterproof sleeve and placed in both your carry‑on and your checked bag. Include the contact details of a local clinic, your doctor’s phone, and the nearest emergency department.
Know the local emergency number (e.g., 000 in Australia, 911 in the US) and have a phrase ready in the local language: “I have asthma, I need an inhaler”. Some countries offer asthma‑specific helplines-bookmark those before you travel.
Gear & Apps That Make a Difference
A pocket‑size Peak Flow Meter measures the fastest speed you can exhale, helping spot worsening asthma early lets you track trends each morning. Record the numbers in a note‑taking app and set alerts if values drop below your personal threshold.
Consider a travel‑specific health app that stores medical info, medication lists, and insurance details. Many of these apps can generate a QR code for quick scanning by emergency responders.
Choosing the Right Inhaler for the Journey
| Inhaler Type | Activation Mechanism | Breath Coordination Needed | Best for Acute Relief | Typical Dose (µg) |
|---|---|---|---|---|
| Metered‑dose inhaler (MDI) | Press‑released spray | Yes - must time inhalation with actuation | Yes | 100‑200 |
| Dry powder inhaler (DPI) | Breath‑activated powder | No - inhalation itself fires the dose | Often used for maintenance | 50‑150 |
| Soft mist inhaler (SMI) | Mechanical spring‑driven mist | Minimal - slower aerosol velocity | Good for both relief and control | 80‑160 |
For most travelers, an MDI with a spacer offers the quickest, most reliable relief, especially during a flight where air turbulence can make precise inhalation tricky. If you prefer a device without coordination demands, a DPI is a solid backup for daily control medication.
Final Checklist Before You Go
- Confirm prescription refill covers the entire trip.
- Pack inhaler, spacer, peak flow meter, saline spray, and a written emergency plan.
- Download AQI and health‑record apps; set daily reminders to check readings.
- Verify travel insurance covers asthma‑related emergencies.
- Brief travel companions on your action plan and where meds are stored.
With these steps, you swap anxiety for confidence and can focus on the sights, sounds, and flavors that make travel unforgettable.
Frequently Asked Questions
Can I bring my inhaler on a plane?
Yes. Carry it in your hand luggage, place it in a clear plastic pouch, and have a doctor’s letter ready if security asks for proof. Most airlines treat inhalers as medical devices.
Do I need a spare inhaler?
Absolutely. Treat it like a passport - lose one and you’re stuck. Pack a duplicate in a separate bag and keep a third in your checked luggage if possible.
How can I check air quality at my destination?
Use free AQI apps such as AirVisual or local government websites. Look for PM2.5 levels below 35µg/m³ for comfortable breathing; higher values may require staying indoors or using a mask.
Is it safe to travel to high‑altitude locations?
High altitude reduces oxygen pressure, which can trigger bronchoconstriction. Acclimatize gradually, keep a rescue inhaler on hand, and monitor peak flow daily. If you have severe asthma, discuss altitude‑specific medication adjustments with your doctor.
Do I need special travel insurance for asthma?
Look for policies that list “pre‑existing respiratory conditions” as covered. Verify that emergency hospital stays, ambulance transport, and medication refills are included.
Can temperature changes worsen my asthma?
Both extreme cold and hot, dry air can irritate airways. Dress in layers, use a scarf over your mouth in cold weather, and keep a humidifier bottle in the hotel room if the air feels dry.



Richard Leonhardt
September 24, 2025 AT 08:52Traveling with asthma can feel scary, but a little planning goes a long way. It’s definatly better to have a plan than to wing it, so keep your rescue inhaler right in your hand‑luggage and make sure it’s in a clear pouch so security doesn’t hold you up. A quick check of the AQI at your destination each morning can save you from an unexpected flare‑up. Remember, a spare inhaler is your best travel buddy, even if it feels like you’re lugging extra weight – it’s worth it.
Shaun Brown
September 26, 2025 AT 16:25Traveling with asthma means you have to treat every flight like a mini‑medical‑checkup.
First, the notion that a simple inhaler will magically fix any altitude‑induced bronchoconstriction is naïve.
You need to understand that cabin pressure drops the partial pressure of oxygen by roughly 20 %.
That reduction alone can trigger a cascade of bronchial hyper‑reactivity in anyone who isn’t obsessively pre‑medicated.
Most travelers think a quick puff will suffice, but the reality is that a pre‑flight dose of a short‑acting beta‑agonist should be taken 15 minutes before boarding.
Skipping that step is equivalent to walking into a thunderstorm without an umbrella.
Second, your so‑called “spare inhaler” isn’t a luxury; it’s a redundancy that most people forget until the first one runs dry.
If you let a single device sit in a checked bag, you’ve already handed yourself a ticket to the emergency department.
Third, the guide’s suggestion to simply “check the AQI” ignores the fact that many popular travel apps pull data from unreliable sources.
You should cross‑reference at least two reputable monitoring services before trusting any single number.
Fourth, portable peak flow meters are touted as “nice to have,” yet without a baseline you’re essentially guessing your own lung capacity.
Establish your personal best and worst values at home, then bring those numbers into the field.
Fifth, the advice to “use a saline spray” is laughably insufficient for the dryness of most jet cabins.
Consider a humidifier mask or a simple misting bottle that can be re‑filled during layovers.
Sixth, the recommendation to “bring a doctor’s letter” is sensible, but most security agents won’t read it even if you hand it over.
In practice, you’re better off memorizing the generic description of your condition and asserting your rights confidently.
Damon Dewey
September 28, 2025 AT 23:58Your checklist reads like a bureaucratic nightmare, but the core advice is solid. Keep it simple and you’ll avoid the drama.
Dan Barreto da Silva
October 1, 2025 AT 07:32Yo, if you think a flight is just a snack break, think again! The cabin air can be a straight‑up assault on your lungs. Pack that spacer like it’s your passport, because without it you’re basically walking on a tightrope with no safety net. And don’t even get me started on hotels that skip HEPA filters – they’re a nightmare for anyone with a bad day. Trust me, you’ll thank me when you’re not wheezing on the runway.
Ariel Munoz
October 3, 2025 AT 15:05Listen, the US has the best medical infrastructure, so if you’re flying from here you already have a leg up. Don’t waste time worrying about obscure foreign clinics when you can just land in Denver, grab a local ER if needed, and be back on the road in no time. Your concerns sound like paranoia, not reality.
Ryan Hlavaty
October 5, 2025 AT 22:38If you skip the spare inhaler, you're basically begging for a disaster.
Chris Faber
October 8, 2025 AT 06:12just grab a cheap air‑purifier for the hostel it’s chill and you won’t even notice the dust the kids in the lobby breathe
aura green
October 10, 2025 AT 13:45Hey, seriously, you’re doing great just by being proactive! 😄 The fact that you’re already checking AQI scores shows you care about your health more than most people care about their phone battery. Keep that emergency plan in a waterproof sleeve – you’ll thank yourself when a sudden storm hits and the hotel’s windows are all shut. And don’t forget the silly little trick of covering your mouth with a scarf in cold weather – it’s like a mini‑heater for your airway. Way to go, traveler, keep the adventure alive! 💪
Edward Morrow
October 12, 2025 AT 21:18Oh, look, another self‑help fluff piece. If you really wanted to survive, you’d stop whining about “feeling great” and actually buy the damn high‑grade spacer that engineers spent years perfecting. This is the kind of half‑hearted advice that belongs in a tourist brochure, not a medical manual.
Shayne Tremblay
October 15, 2025 AT 04:52Hey folks, let’s keep the momentum going! Pack your meds like you’d pack your phone charger – you can’t afford to be without it. A quick daily peak‑flow log can become your personal GPS, pointing you to trouble before it hits. Remember, confidence comes from preparation, not luck. You’ve got this – happy traveling!
Stephen Richter
October 17, 2025 AT 12:25It is advisable to verify that all pharmaceutical devices are stored in accordance with airline regulations. Failure to comply may result in delays at security checkpoints.
Musa Bwanali
October 19, 2025 AT 19:58Right on point, those guidelines are non‑negotiable. If you skip them you’re just asking for trouble, and nobody wants that on a trip.
Allison Sprague
October 22, 2025 AT 03:32Let’s get one thing straight: “just bring a spare inhaler” isn’t a suggestion, it’s a mandate. The grammar in the original guide could use a makeover – there are too many run‑on sentences that could confuse a reader already stressed about asthma. Also, the usage of “definitely” without a proper adverbial clause is sloppy. Precision matters when lives are at stake.
leo calzoni
October 24, 2025 AT 11:05Honestly, the guide tries to sound friendly but ends up sounding like a bored school teacher. Simplicity is key; over‑complicating air‑filter recommendations just confuses travelers with limited budgets.
KaCee Weber
October 26, 2025 AT 17:38🌍 I hear you, but let’s not dismiss those practical tips just because they sound “basic.”🛫 Every traveler, regardless of budget, deserves clear guidance on managing asthma abroad. The emojis are a nice touch, but the core advice-like checking AQI and packing a spare inhaler-remains essential. Keep the positivity flowing! 🚀
jess belcher
October 29, 2025 AT 01:12Travelers should respect local health norms while ensuring their medication is accessible at all times.
Sriram K
October 31, 2025 AT 08:45All in all, an organized checklist, a dependable spare inhaler, and a reliable AQI app are the three pillars of safe travel with asthma. Pair that with a brief conversation with your doctor before you depart, and you’ll minimize surprises. Stay hydrated, keep your spacer handy, and enjoy the journey without fear. Safe travels!
Deborah Summerfelt
November 2, 2025 AT 16:18Isn’t it a bit arrogant to think you can fully control a chronic condition with a checklist? Nature has a way of reminding us who’s really in charge, especially when you’re in a high‑altitude city that refuses to care about your little plan.