Bleeding Complications: Understanding Risks and Management
When dealing with Bleeding Complications, any abnormal loss of blood that can arise from medication, injury, surgery, or internal disease. Also known as hemorrhagic events, they require prompt attention because they can turn a minor issue into a life‑threatening situation. Bleeding complications encompass a range of scenarios—from a nosebleed after a cold to massive internal bleeding after trauma.
One of the biggest drivers is Anticoagulant Therapy, drugs like warfarin, apixaban, and direct oral anticoagulants that thin the blood to prevent clots. While these meds save lives by stopping strokes, they also raise the risk of spontaneous bruising, gastrointestinal bleeding, or bleeding after a minor cut. The relationship is clear: using anticoagulant therapy increases the likelihood of bleeding complications, especially when dosage isn’t carefully monitored. Another frequent source is Surgical Bleeding, excessive blood loss that occurs during or after an operation. Surgeons manage this by using cauterization, hemostatic agents, and vigilant post‑op monitoring. If surgical bleeding isn’t controlled, patients may develop anemia, infections, or delayed wound healing, which then feeds back into the broader category of bleeding complications.
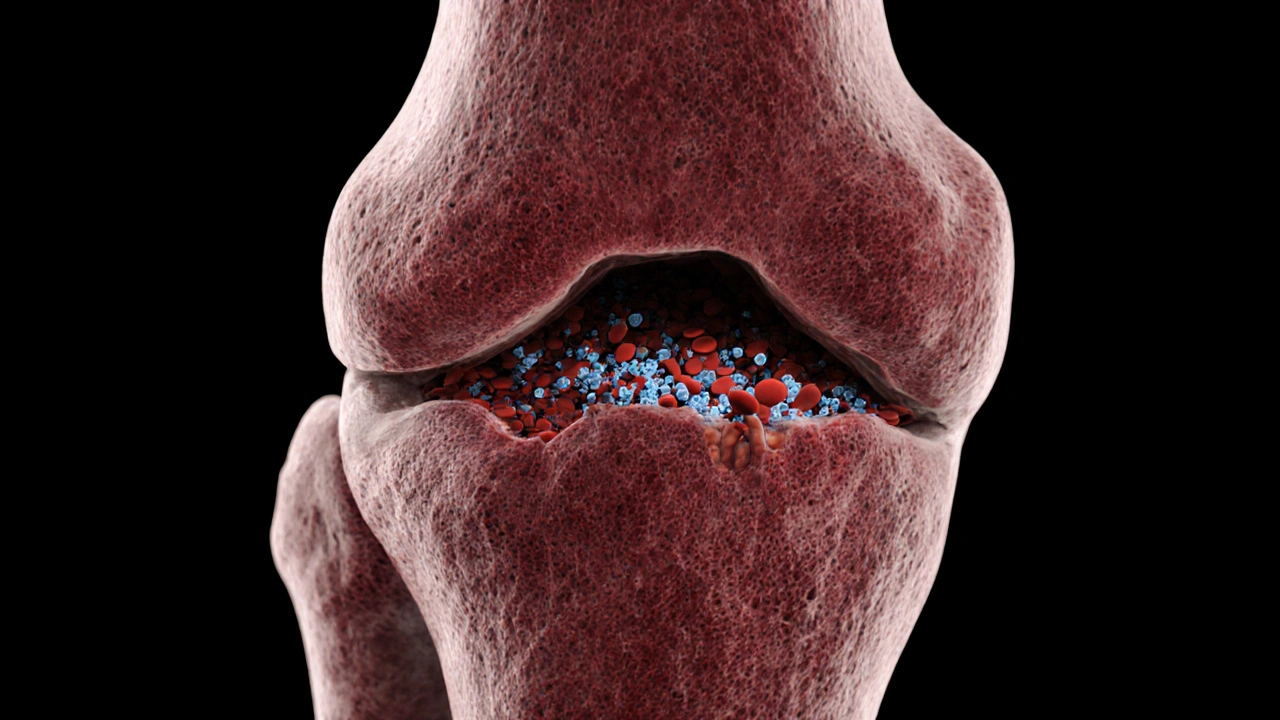
A third major player is Gastrointestinal Bleeding, bleeding that originates in the stomach, intestine, or esophagus, often due to ulcers, NSAIDs, or alcohol use. This type of bleed often shows up as black stools or vomiting blood and can be hidden until it becomes severe. Managing GI bleeding usually involves endoscopic intervention, medication to reduce acid, and sometimes stopping the offending drug. Finally, Trauma‑Induced Bleeding, blood loss caused by accidents, falls, or blunt force injuries illustrates how external forces can trigger internal hemorrhage, especially in patients already on anticoagulants. Trauma’s impact on bleeding complications is a classic cause‑effect chain: injury leads to vessel damage, which, when combined with thin blood, results in rapid blood loss.
Practical Steps to Reduce and Manage Bleeding Risks
Understanding these links helps you act before a crisis. If you’re on anticoagulant therapy, keep regular INR checks or follow your doctor’s lab schedule for newer agents. Pair that with a diet low in vitamin K if you’re on warfarin, and you’ll cut down unexpected spikes. For anyone facing surgery, ask the surgical team about their hemostasis plan and whether you need to pause blood thinners ahead of time. When it comes to gastrointestinal health, limit NSAID use, avoid excess alcohol, and report any unusual stomach pain or dark stools immediately. In the event of trauma, apply direct pressure to visible wounds, elevate the injured limb, and seek emergency care—especially if you’re on blood‑thinning meds, as the bleed can worsen quickly.
All of these strategies tie back to a single goal: keep bleeding complications from escalating. Below you’ll find articles that dive deeper into specific scenarios—whether it’s how age impacts back pain, managing nausea from Alzheimer’s meds, or safely buying generic drugs online. Each piece adds a piece to the puzzle, helping you recognize warning signs, choose the right treatment, and stay in control of your health.
Ready to explore the full collection? Keep reading to discover detailed guidance on medication side effects, post‑surgical care, and everyday habits that protect you from unwanted bleeding.