Bacterial Vaginosis: What It Is and How to Handle It
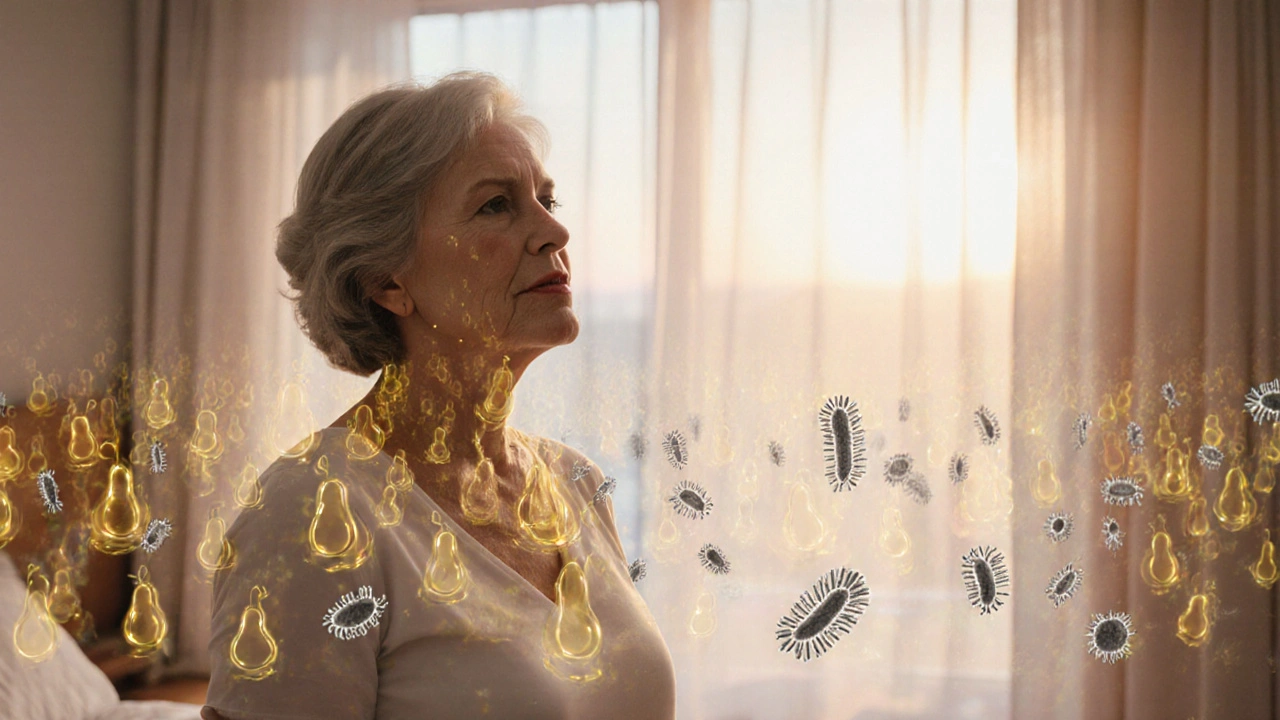
When dealing with bacterial vaginosis, a common vaginal infection caused by an imbalance of natural bacteria. Also known as BV, it can show up as unusual discharge, fishy odor, or mild irritation. Understanding BV helps you spot it early and choose the right care.
One of the biggest players in BV is the vaginal microbiome, the community of good and bad bacteria living inside the vagina. When lactobacilli drop and anaerobes rise, the environment shifts, creating the classic symptoms. This shift requires a treatment plan that restores balance, often starting with antibiotics, drugs that kill harmful bacteria
Key Factors and Management Strategies
Among antibiotics, metronidazole, an oral or gel medication frequently prescribed for BV is the go‑to choice because it targets the anaerobic bugs that cause the problem. A typical course lasts 7 days, and many people feel better within a few days. Some doctors also use clindamycin, another effective option for those who can’t take metronidazole. Both work by reducing the overgrowth of bad bacteria, giving lactobacilli a chance to repopulate.
Antibiotics clear the infection, but recurrence is common. That’s where probiotics, supplements containing live friendly bacteria come into play. Research shows that taking lactobacillus strains after treatment can lower the odds of BV returning. Probiotic foods like yogurt or kefir also help maintain a healthy balance, especially when paired with good hygiene habits.
Lifestyle choices matter too. Avoiding scented soaps, douching, and tight synthetic underwear reduces irritation and keeps the microbiome stable. Some people find that switching to cotton underwear and practicing safe sex—using condoms and limiting the number of partners—lowers the risk of future episodes. Drinking plenty of water and eating a diet rich in fiber support overall gut health, which indirectly benefits vaginal health.
It’s easy to mistake BV for a yeast infection or a sexually transmitted disease because the symptoms overlap. A simple lab test, usually a wet mount or a pH check, tells the difference. BV typically shows a higher pH (above 4.5) and clue cells under the microscope. Knowing the exact cause means you can pick the right medication and avoid unnecessary treatments.
For pregnant women, untreated BV can raise the chance of preterm birth. Doctors often treat BV during pregnancy with metronidazole, which is considered safe in later trimesters. If you’re expecting, talk to your provider about the best plan—early detection is key.
People with diabetes or a weakened immune system should keep an eye on BV because it can be harder to clear. In such cases, a longer antibiotic course or a combination of oral and topical treatments might be recommended. Monitoring symptoms and following up with a healthcare professional ensures the infection doesn’t linger.
If over‑the‑counter remedies don’t work, prescription‑strength options are available. Some clinics offer single‑dose vaginal tablets that combine both an antibiotic and a probiotic, aiming to kill bad bacteria and immediately re‑introduce good ones. These newer formulations are still being studied but show promise for faster recovery.
Remember, BV is not a sign of poor hygiene or a moral failing—it’s a medical condition that many women face at some point. Talking openly with a doctor, getting tested, and following a clear treatment plan can bring quick relief. The articles below dive deeper into specific meds, buying guides, and how to choose the right pharmacy, giving you the tools to manage BV confidently.
Below you’ll find a curated list of resources that break down antibiotic options, safe online purchases, and lifestyle tips—all aimed at helping you tackle bacterial vaginosis head‑on.