BV Risk Assessment Tool for Post-Menopausal Women
Assessment Overview
This tool helps you understand your risk of developing bacterial vaginosis (BV) after menopause. Enter your symptoms and risk factors to get personalized insights.
When a woman hits menopause, the body goes through a cascade of hormonal shifts that can affect everything from bone health to skin texture. One area that often gets overlooked is the vaginal ecosystem, which can become vulnerable to bacterial vaginosis. Understanding why BV tends to flare up during this life stage, how to spot it, and which treatments work best can spare you uncomfortable symptoms and repeated doctor visits.
What Is Bacterial Vaginosis?
Bacterial Vaginosis is a condition where the normal balance of vaginal bacteria is disrupted, leading to an overgrowth of anaerobic organisms such as Gardnerella vaginalis, Mobiluncus, and Mycoplasma hominis. In a healthy vagina, Lactobacillus species dominate, producing lactic acid that keeps the pH below 4.5. When Lactobacilli decline, the pH rises and the anaerobes multiply, causing the characteristic thin, grayish discharge and fishy odor.
BV is not a sexually transmitted infection, but sexual activity can influence the bacterial mix. It’s the most common vaginal complaint in women of reproductive age, affecting up to 29% of them at some point.
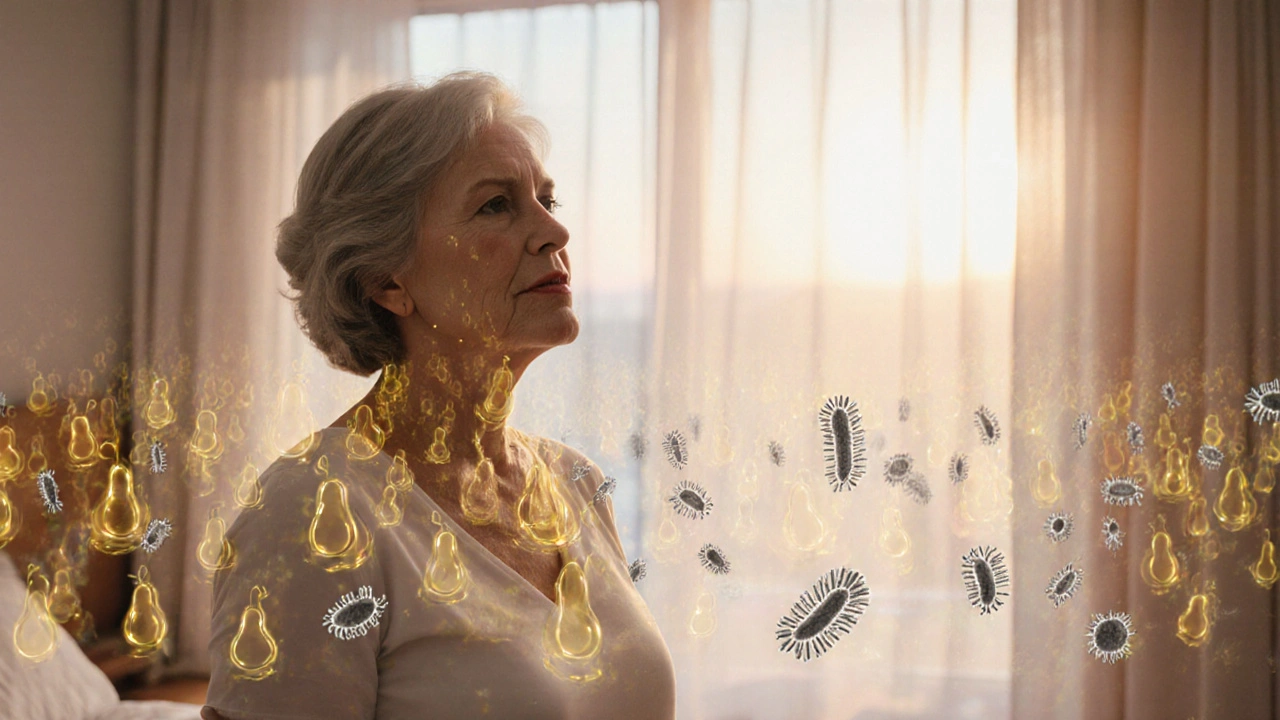
How Menopause Changes the Vaginal Environment
Menopause marks the end of monthly ovarian estrogen production, typically between ages 45 and 55. Estrogen supports the thickness of the vaginal epithelium and the growth of glycogen‑rich cells that feed Lactobacilli. When estrogen drops, the epithelium thins, glycogen levels fall, and Lactobacillus populations shrink.
The resulting rise in vaginal pH creates a more hospitable environment for the anaerobes that cause BV. Studies from 2023-2024 show that post‑menopausal women have a 1.7‑fold higher odds of a BV diagnosis compared with pre‑menopausal peers.
Why BV Becomes More Common After Menopause
- Reduced estrogen: Less glycogen means fewer food sources for Lactobacilli.
- Dryness and irritation: Micro‑tears in the thin epithelium can allow bacteria to shift.
- Changes in sexual activity: New partners or altered lubrication can introduce different bacterial strains.
- Systemic health factors: Diabetes, obesity, and smoking-conditions that rise with age-also increase BV risk.
Because symptoms may be milder or mistaken for normal menopausal dryness, many women delay seeking help, allowing the imbalance to persist.

Recognizing BV Symptoms in Menopausal Women
The classic BV triad-thin gray‑white discharge, a fishy smell, and mild itching-still applies, but there are nuances:
- Discharge volume: May be less noticeable due to overall reduced vaginal secretions.
- Odor intensity: Can become more pronounced after sex or during a warm shower.
- Irritation: Often described as a burning sensation rather than itching.
- Redness: Less common, but can appear if the pH is very high.
If you notice any of these changes lasting more than a few days, it’s worth getting checked.
Getting a Proper Diagnosis
Self‑diagnosis is risky because several conditions-yeast infection, atrophic vaginitis, or even early‑stage cervical changes-can mimic BV. A qualified Gynecologist will typically perform three steps:
- Amsel criteria: Visual inspection of discharge, pH testing (>4.5 supports BV), whiff test with potassium hydroxide, and clue‑cell microscopy.
- Nugent scoring: A lab‑based Gram stain that grades bacterial presence on a 0-10 scale; scores of 7-10 confirm BV.
- Exclusion of other causes: Wet mount analysis to rule out Candida or Trichomonas.
Because the vaginal flora can fluctuate, a single test might miss BV. If symptoms linger, ask for a repeat test.
Treatment Options: What Works Best for Post‑Menopausal Women?
First‑line therapy remains oral or vaginal antibiotics, but the menopausal context adds extra considerations such as drug interactions and bone health.
Antibiotics
- Metronidazole 500mg orally twice daily for 7days (or 0.75% gel applied nightly for 5days). Effective in >85% of cases, but recurrence rates can reach 30% within three months.
- Clindamycin 300mg orally twice daily for 7days. Useful for metronidazole‑intolerant patients; may cause yeast overgrowth.
Both drugs can interact with warfarin and certain antidepressants, so disclose all meds to your doctor.
Adjunctive Probiotics
- Oral LactobacillusrhamnosusGR‑1 and L.reuteriRC‑14 (one capsule daily for 30days) have shown a 40% reduction in recurrence when paired with antibiotics.
- Vaginal probiotic suppositories (e.g., Lactin-V) are emerging as a promising maintenance strategy, though they’re not yet covered by Australian PBS.
Because estrogen deficiency hampers Lactobacillus re‑colonization, many clinicians now combine low‑dose topical estrogen with antimicrobial therapy for women with severe atrophy.
Comparing Antibiotics and Probiotics
| Attribute | Antibiotics (Metronidazole/Clindamycin) | Probiotics (Oral or Vaginal) |
|---|---|---|
| Initial cure rate | 80‑90% | 30‑40% (as sole therapy) |
| Recurrence within 3months | 25‑35% | 15‑20% (when used after antibiotics) |
| Side effects | Nausea, metallic taste, possible yeast overgrowth | Generally mild; occasional bloating |
| Interaction risk | High (warfarin, alcohol) | Low |
| Convenience | 7‑day regimen | 30‑day regimen |
For most menopausal women, the best approach is a short course of antibiotics followed by a probiotic maintenance plan, especially if you’ve experienced multiple recurrences.
Prevention Strategies Tailored to Menopause
- Maintain vaginal moisture: Regular use of water‑based lubricants during intercourse reduces micro‑tears.
- Wear breathable fabrics: Cotton underwear and loose‑fitting clothes keep the area dry and discourage anaerobic growth.
- Avoid douches and scented products: They strip protective mucus and disrupt pH.
- Balanced diet: Foods rich in prebiotic fibers (e.g., garlic, onions, bananas) support Lactobacillus growth.
- Consider low‑dose vaginal estrogen: A 10‑microgram estradiol tablet inserted twice weekly restores glycogen and lowers BV risk.
- Regular screenings: Annual pelvic exams help catch imbalances early, especially if you have diabetes or are a smoker.
When to See a Gynecologist Immediately
If you experience any of these, schedule an appointment promptly:
- Severe burning or pain during urination.
- Fever or pelvic pain, which could signal a spreading infection.
- Recurring BV after two standard antibiotic courses.
- Bleeding after intercourse, which may indicate atrophic changes or other pathology.
Early intervention prevents complications such as pelvic inflammatory disease, which can affect fertility even after menopause.
Quick Checklist for Managing BV During Menopause
- Know the symptoms: discharge, odor, mild irritation.
- Get a proper diagnosis - Amsel criteria or Nugent score.
- Follow a prescribed antibiotic course fully.
- Start a probiotic regimen within 48hours of finishing antibiotics.
- Consider topical estrogen if you have chronic dryness.
- Adopt daily hygiene habits: cotton underwear, no douching.
- Schedule a follow‑up exam within one month.
Frequently Asked Questions
Can I get BV from my partner?
BV isn’t classified as a classic STI, but a partner can change the bacterial mix through intercourse. Using condoms and avoiding vaginal intercourse when either partner has symptoms reduces the risk.
Is over‑the‑counter (OTC) treatment effective?
OTC antifungal creams won’t treat BV because the cause is bacterial, not fungal. Some OTC probiotic gels may help after a prescription course, but they shouldn’t replace antibiotics.
How long does it take for the vagina to return to a healthy state?
After completing antibiotics, most women see symptom relief within a few days. Full restoration of a Lactobacillus‑dominant flora can take 2‑4weeks, especially if you’re also using probiotics or estrogen.
Will hormone replacement therapy (HRT) prevent BV?
Systemic HRT can improve overall vaginal health, but the evidence for BV prevention is mixed. Local vaginal estrogen has a clearer benefit for restoring Lactobacilli and lowering pH.
Is BV linked to urinary tract infections (UTIs)?
Yes. The same bacterial imbalance that causes BV can also promote E.coli growth, raising the chance of a UTI. Treating BV often reduces recurring UTIs.

Jason Ring
October 10, 2025 AT 14:41Ths article trully highlights th challenges.
Kelly Hale
October 11, 2025 AT 10:08Reading about bacterial vaginosis in the twilight of our reproductive years feels like stepping onto a stage where the curtains have already been drawn, yet the drama unfolds with relentless intensity. Menopause, that inevitable hormonal apocalypse, strips away the protective veil of estrogen, leaving the vaginal ecosystem exposed like a battlefield after a siege. The once‑dominant Lactobacilli, those humble guardians of acidity, are forced into retreat, and in their absence, the opportunistic anaerobes march forward with a sinister confidence. This microbial rebellion manifests as the thin, gray‑white discharge that haunts many women, accompanied by a fishy perfume that lingers like a bad memory after intimacy.
But the story does not end with symptoms; it spirals into the realm of diagnosis, where the Amsel criteria and Nugent scoring become the judges of truth. Physicians, armed with pH strips and microscopes, must decipher whether the culprit is truly BV or an impostor like Candida, each demanding a distinct therapeutic script. The prescribed antibiotics-metronidazole or clindamycin-act as swift but sometimes fleeting cavalry, clearing the field only to watch it be repopulated within weeks.
Enter the probiotic allies, the microscopic reinforcements that promise lasting peace. Yet their efficacy is a saga of its own, contingent upon timing, dosage, and the patient's willingness to adhere to a month‑long regimen. Meanwhile, the subtle specter of estrogen deficiency looms, suggesting that low‑dose vaginal estrogen may be the keystone in restoring the Lactobacilli stronghold.
Beyond pharmacology, lifestyle adjustments whisper their counsel: breathable cotton, avoidance of scented intruders, and the judicious use of lubricants to prevent micro‑tears. Each recommendation is a thread in the tapestry of prevention, weaving together diet, hygiene, and sexual health. For those grappling with diabetes, obesity, or smoking, the stakes are amplified, as these systemic factors fan the flames of dysbiosis.
In the grand theater of women's health, BV after menopause is not merely a footnote but a compelling act that demands attention, empathy, and a multidisciplinary chorus of solutions.
Neviah Abrahams
October 12, 2025 AT 05:34The article is solid but I think it overlooks the psychological toll of recurrent infections and how that can affect compliance with treatment protocols. Women often feel embarrassed and may delay seeking help which only worsens the situation. Also the piece could have mentioned the role of biofilm formation in BV persistence which is a key factor many clinicians ignore.
Uju Okonkwo
October 13, 2025 AT 01:01Hey everyone, just wanted to add that staying hydrated and incorporating fermented foods like yogurt or kefir can naturally boost Lactobacilli levels. Also, regular pelvic exams are crucial-don’t skip them because you think "it’s just menopause". Small steps daily can make a big difference in keeping the vaginal flora balanced.
Angie Robinson
October 13, 2025 AT 20:28Honestly this article is way too generic; it doesn’t address the real-world frustrations of dealing with recurring BV while juggling work and family. The tone feels bland and the advice is obvious-who needs another reminder to wear cotton underwear?
Emmons Kimery
October 14, 2025 AT 15:54Great breakdown! 👍 Remember to finish the full antibiotic course, then start probiotics within 48 hours. 🎯 If you’re comfortable, discuss low‑dose vaginal estrogen with your doctor-it can really help restore the pH. 💡 Stay proactive and keep track of any changes.
Mimi Saki
October 15, 2025 AT 11:21Thanks for the info! 😊 Keeping a symptom diary can help you and your doc see patterns. 🌸 And don’t forget to hydrate and eat plenty of fiber-it supports overall gut health, which ties back to vaginal health.
Subramaniam Sankaranarayanan
October 16, 2025 AT 06:48From a clinical perspective, it’s essential to recognize that BV is not a simple infection but a dysbiosis driven by ecological imbalance. The drop in estrogen reduces glycogen, which in turn deprives Lactobacilli of their primary substrate, allowing anaerobes to dominate. Empirical treatment with metronidazole remains first‑line, yet the recurrence rate underscores the need for adjunctive strategies. Probiotics, particularly strains like L. rhamnosus GR‑1, have demonstrated efficacy in re‑establishing a protective microbiota when administered post‑antibiotic. Moreover, low‑dose vaginal estrogen not only restores mucosal thickness but also improves glycogen deposition, providing a substrate for beneficial bacteria. Clinicians should adopt a multimodal approach, tailoring therapy to each patient’s comorbidities, such as diabetes, which can further predispose to BV. Regular follow‑up is crucial; a single negative Nugent score does not guarantee lasting remission.
Kylie Holmes
October 17, 2025 AT 02:14Wow, this is super helpful! Can’t wait to share it with my mom-she’s going through menopause now and could use the tips.
Jennifer Wees-Schkade
October 17, 2025 AT 21:41Important to note: if symptoms persist after two courses of antibiotics, consider a referral to a specialist for possible alternative therapies or evaluation for co‑existing conditions. Always verify drug interactions, especially with anticoagulants.
Fr. Chuck Bradley
October 18, 2025 AT 17:08Great info!