Akathisia vs. Restless Legs Symptom Checker
Understand Your Symptoms
This tool helps you distinguish between akathisia and restless legs syndrome (RLS), two conditions that can be confused but require different treatments.
Answer These Questions
Imagine sitting still for just five minutes-your legs feel like they’re crawling with ants, your body aches to move, and no matter how much you shift, you can’t find relief. You tell your doctor you’re anxious. They up your antidepressant. The restlessness gets worse. You start having thoughts you never had before. This isn’t anxiety. It’s akathisia-a dangerous, often missed side effect of common medications.
What Exactly Is Akathisia?
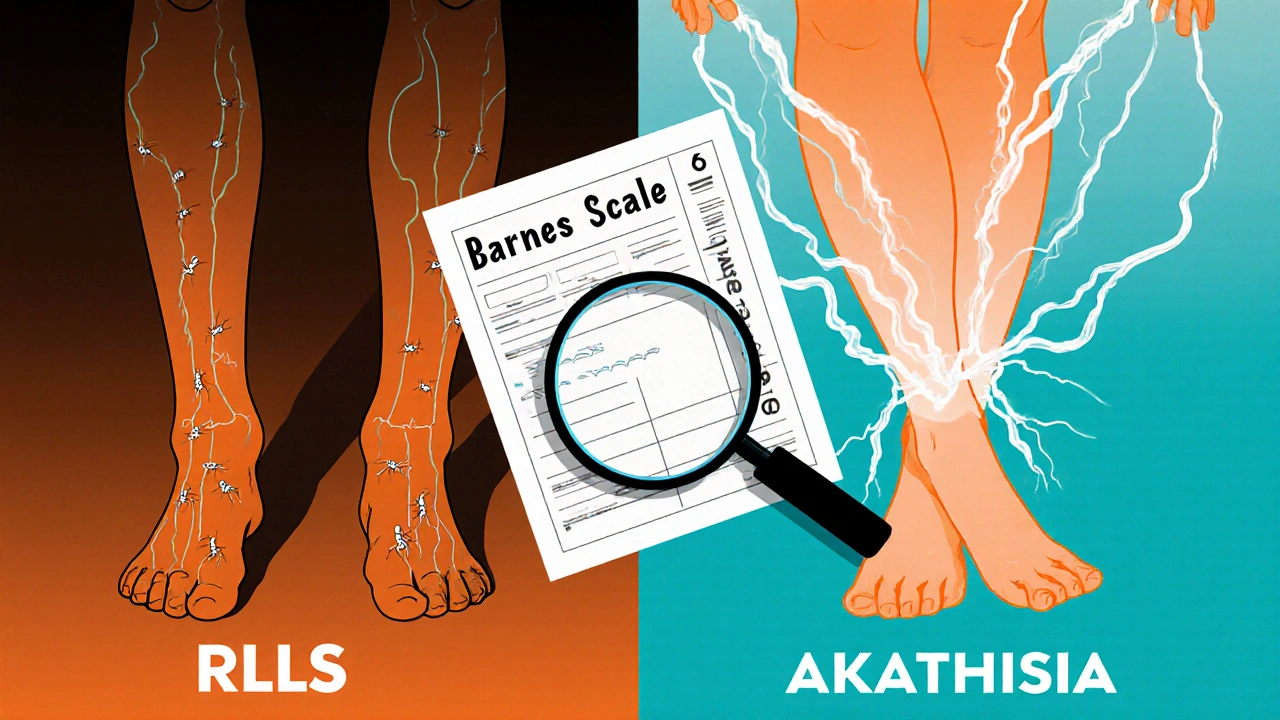
Akathisia isn’t just feeling fidgety. It’s a movement disorder caused by medications, most often antipsychotics like haloperidol, risperidone, or even older antidepressants and anti-nausea drugs like metoclopramide. First identified in the 1950s, it’s one of the most common side effects of these drugs, affecting up to 40% of people on first-generation antipsychotics and 5-15% on newer ones. The key sign? An unbearable urge to move, especially when sitting. People describe it as an internal burning, aching, or electric current that demands motion. You might cross and uncross your legs repeatedly, rock back and forth, pace in place, or shift your weight constantly. Unlike normal restlessness, this isn’t something you can ignore. It’s physically painful and emotionally terrifying. And here’s the trap: doctors often mistake it for worsening anxiety or agitation. That leads to the worst possible response-increasing the very medication causing the problem. A 2017 case study in Australia documented a patient who developed suicidal thoughts after their haloperidol dose was doubled because the doctor thought they were “more psychotic.” The symptoms vanished within three days of stopping the drug.How Is Akathisia Different From Restless Legs Syndrome?
Restless legs syndrome (RLS) and akathisia sound similar. Both make you want to move your legs. But they’re not the same-and mixing them up can be deadly. RLS happens mostly at night or when you’re resting. It’s a creepy-crawly feeling in the calves or feet that improves with movement. It often runs in families and can be linked to low iron or kidney disease. Treatment usually involves dopamine-boosting drugs like ropinirole or pramipexole. Akathisia? It hits anytime you’re still-sitting in a chair, watching TV, even during a doctor’s appointment. The urge isn’t localized to the legs; it’s full-body. You feel like you’re going to explode if you don’t move. And here’s the critical difference: dopamine medications that help RLS can make akathisia much worse. A 2022 study in the Journal of Clinical Psychiatry found that nearly 70% of patients with medication-induced restlessness were initially diagnosed with RLS or anxiety. Only after switching doctors or doing their own research did they learn it was akathisia.Which Medications Cause Akathisia?
Not all drugs cause it equally. The biggest culprits are:- First-generation antipsychotics: Haloperidol, fluphenazine, chlorpromazine. These have the highest risk because they strongly block dopamine receptors.
- Second-generation antipsychotics: Risperidone, aripiprazole, olanzapine. Lower risk than first-gen, but still common-especially at higher doses.
- Anti-nausea drugs: Metoclopramide (Reglan) and prochlorperazine. Used for migraines or stomach issues, these can trigger akathisia even in people without psychiatric conditions.
- Some antidepressants: SSRIs like fluoxetine or sertraline, especially when started or increased quickly.
How Doctors Diagnose It (And Why They Often Miss It)
There’s a simple, 5-minute tool called the Barnes Akathisia Rating Scale (BARS). It asks two things:- How intense is your inner feeling of restlessness? (0 = none, 3 = severe)
- How much are you moving your legs or body? (0 = none, 3 = constant pacing)
How to Treat It
The first rule? Don’t add more meds. Stop the one causing it-if you can. If the medication is essential (like for severe psychosis), here’s what works:- Reduce the dose: Even a small drop can help. Haloperidol should be tapered over 3-5 days to avoid withdrawal.
- Switch medications: Move from haloperidol to quetiapine or clozapine-both have lower akathisia risk.
- Add propranolol: A beta-blocker like propranolol (10-20 mg twice daily) reduces the physical urge to move. It’s often the first add-on treatment.
- Try clonazepam: A low dose (0.5-1 mg at night) can calm the nervous system. But don’t use long-term-it’s addictive.
- Cyproheptadine: An antihistamine that blocks serotonin. Works for some, especially if SSRIs triggered it.
What You Can Do Right Now
If you’re on any of these medications and feel restless:- Write down when the symptoms started-did they begin after a dose increase?
- Track when they’re worst: sitting? At night? After meals?
- Ask your doctor: “Could this be akathisia?” Show them the Barnes Scale.
- Don’t accept “it’s just anxiety.” Push for a medication review.
- If you’re having suicidal thoughts, tell someone immediately. This is a medical emergency.
The Bigger Problem: Why This Keeps Happening
Akathisia isn’t rare. It’s ignored. Only 37% of U.S. psychiatric clinics screen for it routinely. Many doctors still think it’s “just behavioral.” But the science is clear: this is a brain reaction to dopamine disruption. It’s not in your head-it’s in your neurons. New tools are emerging. In 2023, the International Parkinson and Movement Disorder Society launched an app that helps clinicians spot akathisia from video calls. Stanford’s AI system can now detect the subtle leg movements from a phone camera with 89% accuracy. But until every doctor learns to ask the right question, people will keep suffering.Final Thought: Your Body Is Trying to Tell You Something
If you’re on a psychiatric or anti-nausea medication and you can’t sit still, don’t blame yourself. Don’t assume it’s stress. Don’t let someone tell you it’s “all in your head.” Akathisia is real. It’s treatable. And it’s preventable-if you speak up.Can akathisia go away on its own?
Sometimes, yes-but only if you stop or reduce the medication causing it. If you keep taking the drug, akathisia usually gets worse. In some cases, it becomes chronic and lasts for months or even years after stopping the drug. That’s why early recognition is critical.
Is akathisia the same as anxiety?
No. Anxiety is a mental state-worry, fear, racing thoughts. Akathisia is a physical urge to move caused by brain chemistry changes. You can have both at the same time, but treating anxiety with more medication won’t fix akathisia. In fact, it often makes it worse.
Can antidepressants cause akathisia?
Yes. SSRIs like sertraline, fluoxetine, and escitalopram can trigger akathisia, especially when starting or increasing the dose. It’s less common than with antipsychotics, but still happens in up to 10% of users. If you feel restless after starting an SSRI, tell your doctor.
What’s the fastest way to relieve akathisia?
The fastest relief usually comes from stopping the causative drug-especially if it’s a first-generation antipsychotic like haloperidol. If you can’t stop it, adding propranolol (10-20 mg) can reduce symptoms within 24-48 hours. Clonazepam also works quickly but carries risks of dependence.
Are there any natural remedies for akathisia?
There’s no strong evidence that herbs, supplements, or diet changes fix akathisia. Some people report mild relief from magnesium or vitamin B6, but these don’t replace medical treatment. The root cause is medication-induced dopamine disruption-so the solution is adjusting meds, not supplements.
Can akathisia lead to suicide?
Yes. Studies show akathisia is linked to increased suicidal thoughts, aggression, and violence. The distress is so intense that some patients say they’d rather return to psychosis than keep living with it. If you or someone you know has akathisia and is having suicidal thoughts, seek emergency help immediately.
How long does akathisia last?
It depends. Acute akathisia lasts less than 6 months and often resolves after stopping the drug. Chronic akathisia lasts longer than 6 months and may persist even after discontinuation. Tardive akathisia can appear months or years later and is harder to treat. Early action gives you the best chance of full recovery.
Should I stop my medication if I think I have akathisia?
Never stop psychiatric medication suddenly without medical supervision. Doing so can cause withdrawal seizures, psychosis rebound, or worsen symptoms. Instead, talk to your doctor. They can help you taper safely or switch to a lower-risk drug while managing your symptoms.



Cynthia Boen
November 27, 2025 AT 08:46This article is garbage. I’ve been on sertraline for two years and I’ve never felt this ‘crawling’ nonsense. People just want to blame drugs because they don’t want to face their own anxiety. Stop medicalizing normal discomfort.
Amanda Meyer
November 28, 2025 AT 16:40I appreciate the clinical detail here, but I’m disturbed by how often this is dismissed. I had a cousin on haloperidol who developed severe akathisia-she was told she was ‘resisting treatment.’ She ended up in the ER after trying to climb out a window. This isn’t theoretical. It’s systemic negligence. The Barnes Scale should be mandatory in all psychiatric intake forms. Period.
Jesús Vásquez pino
November 30, 2025 AT 12:06Yo, I’ve been there. Took metoclopramide for reflux and suddenly couldn’t sit still for shit. Went to my doc, he laughed. Said I was ‘too high-energy.’ Two months later I was pacing my apartment at 3 a.m., crying because I felt like my bones were vibrating. Finally found a neurologist who knew what it was. Propranolol saved me. If you’re on anything that blocks dopamine and feel like you’re trapped in a Tesla coil-listen to yourself. Don’t let a lazy doctor gaslight you.
hannah mitchell
December 1, 2025 AT 00:49Thanks for posting this. I’ve been too scared to say anything because I thought I was just ‘high-strung.’ Now I’m going to print out the Barnes Scale and bring it to my next appointment. I’ve been on risperidone for six months and I’ve been rocking back and forth so much my chair’s squeaking.
vikas kumar
December 1, 2025 AT 02:59As someone from India who’s seen both traditional and Western medicine, I can say this: akathisia is ignored everywhere. In my village, people just say ‘he’s possessed.’ In hospitals, they say ‘it’s depression.’ No one looks at the meds. I’ve trained nurses here to ask three simple questions: When did it start? Does it happen when sitting? Does movement help? It’s not rocket science. Just common sense.
Vanessa Carpenter
December 1, 2025 AT 11:13I’ve had RLS since I was 18. Took ropinirole for years. Then I started sertraline for panic attacks. Suddenly, I couldn’t sit through a movie. My legs weren’t just crawling-they felt like they were on fire. I thought it was RLS flaring. Turned out it was akathisia. Stopped the SSRI, added propranolol, and the burning stopped. I wish I’d known this sooner. Thank you for writing this.
Ginger Henderson
December 2, 2025 AT 04:16Wait, so antidepressants cause this? But my therapist says SSRIs are ‘safe and effective.’ What if this is just a scam to sell more drugs? Maybe the real problem is that people are too lazy to meditate or do yoga? Just saying.
Bethany Buckley
December 3, 2025 AT 15:20While the phenomenological description of akathisia is compelling, the epistemological framework underpinning this article remains dangerously reductionist. The conflation of neurochemical disruption with somatic symptomatology risks reifying a biomedical hegemony that pathologizes embodied subjectivity. Moreover, the uncritical endorsement of propranolol as a panacea neglects the hermeneutic dimensions of patient experience. One must interrogate not only dopamine blockade-but the ontological violence of institutionalized psychiatry.
Douglas Fisher
December 4, 2025 AT 21:49I’ve been reading this whole thing, and I just want to say-I’m so sorry anyone has to go through this. I had a friend who went undiagnosed for 14 months. She stopped sleeping. She stopped eating. She stopped talking. And every time she said, ‘I can’t sit still,’ they just gave her more meds. Please, if you’re reading this and you feel this way-don’t wait. Write down the dates. Take the Barnes Scale. Show it to someone who listens. You’re not crazy. You’re not lazy. You’re not anxious. You’re being poisoned by a drug that was supposed to help. And you deserve better.
stephen riyo
December 6, 2025 AT 07:21My sister’s on olanzapine… and she’s been pacing like a caged tiger since January. I showed her this article. She cried. She’s finally going to ask her psychiatrist to reduce the dose. I’m so glad someone finally put this into words. Thank you.