Antidepressant Tapering Calculator
Create Your Personalized Tapering Plan
Based on current clinical guidelines for safe antidepressant discontinuation
Your Personalized Tapering Schedule
Important Notes
Do not reduce faster than recommended—this significantly increases withdrawal symptoms. If you experience severe symptoms, pause and consult your doctor.
Pro Tip: For the final 10% of your taper, consider micro-tapering (reductions of 1-2mg) for safer discontinuation.
Stopping antidepressants isn’t as simple as skipping a pill. For many people, even a small reduction can trigger dizziness, brain zaps, nausea, or intense anxiety-not because their depression is coming back, but because their brain is adjusting to lower drug levels. This is called antidepressant discontinuation syndrome, and it affects between 27% and 86% of people who stop abruptly. The good news? You don’t have to suffer through it. With the right tapering plan, most withdrawal symptoms can be avoided or greatly reduced.
Why Tapering Matters More Than You Think
Antidepressants work by changing how your brain handles neurotransmitters like serotonin. When you take them regularly, your brain adapts. Suddenly removing the drug leaves your brain out of balance. That’s when symptoms show up: electric shock-like sensations in the head (often called ‘brain zaps’), nausea, insomnia, irritability, or even flu-like body aches. These aren’t signs of relapse-they’re signs of withdrawal. A 2022 Harvard study of over 400 patients found that those who stopped their medication in under a week had a 32% chance of relapsing within six months. Those who tapered slowly over two weeks or more cut that risk to 19%. That’s a 40% drop in relapse risk just from slowing down the process. And it’s not just about avoiding depression returning. Withdrawal symptoms can be so severe that nearly 73% of people mistake them for their depression coming back-and end up restarting medication unnecessarily. Knowing the difference saves time, money, and emotional stress.Not All Antidepressants Are the Same
The half-life of your medication-how long it stays active in your body-determines how fast you can taper. Shorter half-life drugs leave your system quickly, which means your brain feels the drop faster. That’s why some medications need much slower tapers than others.- Short half-life (need slow taper): Paroxetine (21 hours), sertraline (26 hours), venlafaxine (13 hours). These are the most likely to cause withdrawal symptoms. Paroxetine, for example, causes symptoms in 44% of people who quit cold turkey.
- Long half-life (can taper faster): Fluoxetine (2-4 days for its active metabolite). Because it lingers, fluoxetine often causes fewer withdrawal symptoms. Some people can stop it abruptly without issues, but even then, a slow taper is still safer.
- MAO inhibitors: These require a 14-21 day washout period before switching to any other antidepressant. Jumping from an MAOI to an SSRI too soon can cause serotonin syndrome-a dangerous, sometimes fatal condition.
How to Taper: Step-by-Step Schedules
There’s no one-size-fits-all plan. But here are proven methods based on clinical guidelines from Australia, the UK, and the US.General Rule: Reduce by 10-25% Every 1-4 Weeks
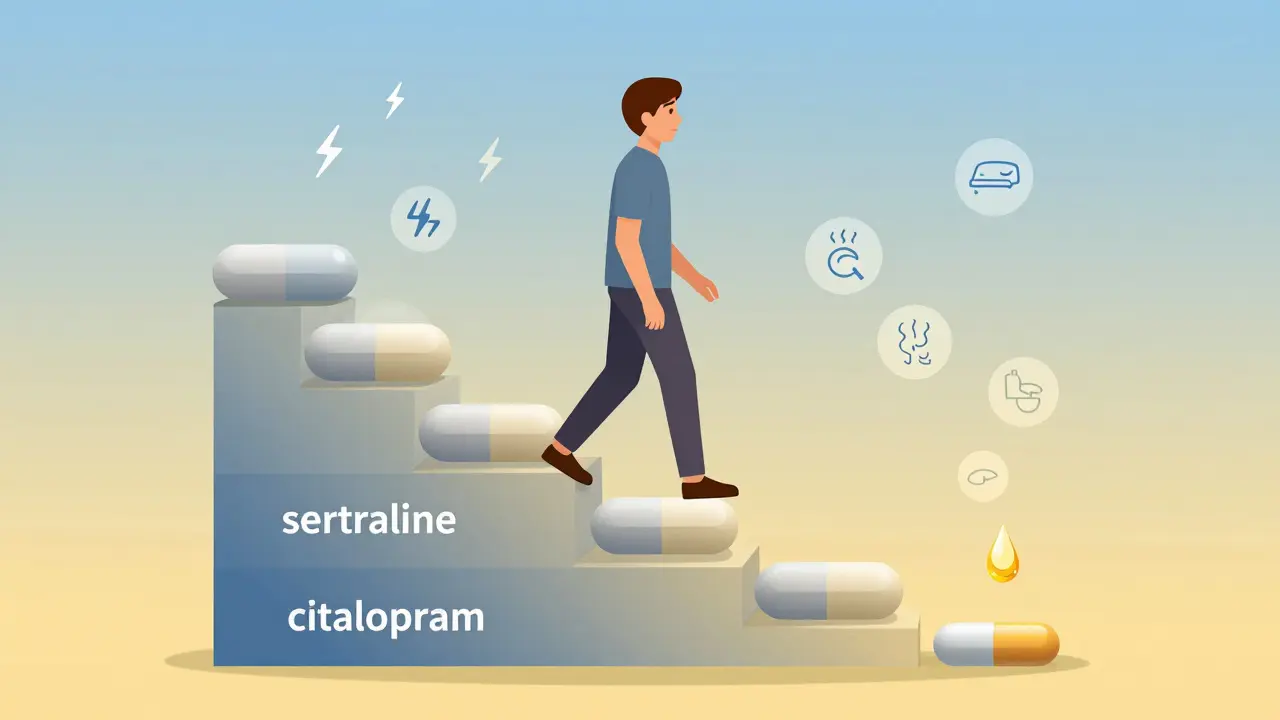
Start by cutting your daily dose by 10% to 25%. Wait at least one week before the next reduction. If you feel fine, wait two to four weeks. If symptoms appear, pause the taper and stay at the current dose until they settle-sometimes that takes days, sometimes weeks. For example:- You’re on citalopram 20mg daily. Reduce to 15mg for two weeks. Then drop to 10mg for two weeks, then 5mg for two weeks, then stop.
- You’re on sertraline 100mg. Reduce to 75mg for three weeks, then 50mg for three weeks, then 25mg for four weeks, then stop.
The Last 10% Is the Hardest
Psychiatrist Dr. David Healy calls this the ‘last 10% problem.’ Even though you’re only reducing the final 10% of your dose, it causes about half of all withdrawal symptoms. Why? Because your brain’s serotonin receptors are hypersensitive by then. A 5mg drop that was fine at the start can now feel like a 20mg drop. That’s why experts now recommend micro-tapering for the final stages:- Switch to a liquid formulation (available for sertraline, citalopram, escitalopram). This lets you reduce by 1mg at a time.
- Use pill splitters for tablets (only if the pill is scored and designed for splitting).
- Reduce by 5-10% every 1-2 weeks during the last quarter of your taper.
Switching Antidepressants? Use Cross-Tapering
If you’re switching from one antidepressant to another, don’t stop the old one and wait. Instead, overlap them. Example: Switching from venlafaxine to sertraline.- Week 1-2: Reduce venlafaxine by 37.5mg every 3-7 days. Increase sertraline by 25mg every 3-7 days.
- By week 4: Venlafaxine is at 0mg. Sertraline is at your target dose.
What to Watch For
Withdrawal symptoms usually start within a few days of reducing your dose. They peak around day 3-5 and fade within 1-2 weeks if you’re tapering correctly. Common symptoms include:- Brain zaps (electric shock feelings in the head)
- Dizziness or vertigo (reported in 63% of cases)
- Nausea, vomiting, or diarrhea
- Flu-like symptoms (fatigue, muscle aches-45% of cases)
- Sensory changes (tingling, light sensitivity-37% of cases)
- Insomnia or vivid dreams
- Anxiety or mood swings
Who Needs Extra Care?
Some people are at higher risk for tough withdrawals:- Long-term users (5+ years): Their brains have adapted more deeply. Withdrawal can last weeks or months. Tapers should be slower-often 3-6 months.
- Those who’ve had withdrawal before: If you’ve had bad symptoms in the past, your next taper should be even slower. Micro-tapering is essential.
- People with anxiety disorders: Withdrawal can mimic panic attacks. A slow taper helps avoid triggering them.
- Older adults: Slower metabolism means drugs stay longer. Tapering too fast can cause confusion or falls.
What Doesn’t Work
Avoid these common mistakes:- Stopping cold turkey. Even if your doctor says it’s okay, it’s risky. Fluoxetine is the only exception-and even then, a slow taper is still safer.
- Using herbal supplements to ‘ease’ withdrawal. St. John’s Wort can interact dangerously with antidepressants. No natural remedy has been proven to prevent withdrawal symptoms.
- Skipping check-ins. Tapering isn’t a DIY project. Regular check-ins with your prescriber help catch problems early.
- Waiting until you feel ‘ready’ to start. If you’re feeling stable, that’s the best time to begin. Waiting until you’re stressed or overwhelmed makes withdrawal worse.

What’s New in Tapering (2025)
Guidelines are finally catching up with what patients have been saying for years.- Micro-tapering is now mainstream. The 2022 TRED guideline recommends reducing by 5-10% every 1-2 weeks during the final 25% of the taper.
- Liquid formulations are being promoted. More pharmacies now stock liquid versions of SSRIs for precise dosing.
- Genetic testing is emerging. Early studies show CYP2D6 and CYP2C19 gene variants predict how fast you metabolize antidepressants-and how bad your withdrawal might be. Testing isn’t routine yet, but it’s coming.
- Guidelines are getting specific. The Maudsley Prescribing Guidelines now list exact milligram reductions for 17 different antidepressants. That’s a big step forward.
When to Pause or Stop
You’re not failing if you need to slow down. In fact, slowing down is often the smartest move. Pause your taper if:- Symptoms last more than two weeks.
- You feel worse, not better, after a reduction.
- You’re having suicidal thoughts or severe anxiety.
Final Advice
Tapering isn’t a race. It’s a careful dance between your brain and your medication. The goal isn’t to stop as fast as possible-it’s to stop without losing your stability. Work with your doctor. Use liquid formulations if you can. Track your symptoms in a journal. Be patient with yourself. And remember: you’re not weak for needing time. You’re smart for listening to your body.How long does antidepressant withdrawal last?
For most people, withdrawal symptoms last 1-4 weeks if the taper is gradual. But for those on short-half-life drugs or who tapered too fast, symptoms can last 6-8 weeks. In rare cases, especially with long-term use, symptoms can persist for months-this is called protracted withdrawal. Slowing the taper reduces the risk of this happening.
Can I taper without my doctor’s help?
Technically, yes-but it’s not recommended. Antidepressants affect brain chemistry, and withdrawal can be unpredictable. A doctor can help you choose the right taper speed, adjust for your specific medication, monitor for complications, and recognize if symptoms are withdrawal versus relapse. Most cases of severe withdrawal happen when people taper on their own.
Is it safe to use pill splitters for tapering?
Only if the tablet is scored and designed for splitting. Not all antidepressants can be split evenly. For example, extended-release capsules or tablets with coatings should never be split. For precise reductions, liquid formulations are far more reliable. Ask your pharmacist if your medication can be safely split.
Why do I feel worse after reducing my dose even though I’m not depressed?
That’s likely antidepressant discontinuation syndrome, not depression returning. Your brain is adjusting to lower drug levels. Symptoms like brain zaps, dizziness, and anxiety are neurological, not emotional. They’re temporary and will fade if you hold your dose for a few weeks. If you’re unsure, track your symptoms and talk to your doctor.
Are there any medications to help with withdrawal symptoms?
There’s no FDA-approved drug for antidepressant withdrawal. Some doctors prescribe short-term low-dose benzodiazepines for severe anxiety or insomnia, but these aren’t meant for long-term use. Sleep aids or anti-nausea meds may help temporarily. The best treatment is time and a slower taper. Avoid herbal remedies like St. John’s Wort-they can interact dangerously.


Payton Daily
December 27, 2025 AT 22:07Kelsey Youmans
December 29, 2025 AT 13:22Sydney Lee
December 30, 2025 AT 20:14oluwarotimi w alaka
December 31, 2025 AT 07:46Debra Cagwin
January 2, 2026 AT 05:54Hakim Bachiri
January 3, 2026 AT 02:28Celia McTighe
January 5, 2026 AT 01:45Ryan Touhill
January 6, 2026 AT 22:05Teresa Marzo Lostalé
January 8, 2026 AT 08:36ANA MARIE VALENZUELA
January 9, 2026 AT 08:26Bradly Draper
January 10, 2026 AT 11:00Gran Badshah
January 10, 2026 AT 12:09Ellen-Cathryn Nash
January 12, 2026 AT 02:19