Parkinson's treatment: Practical options, medicines, and everyday tips
Parkinson's disease changes movement, mood, and daily routine. If you or someone you care about has Parkinson's, knowing treatment options helps you make better choices. This page collects practical advice on medications, therapies, and safety tips so you can act with confidence.
Medications
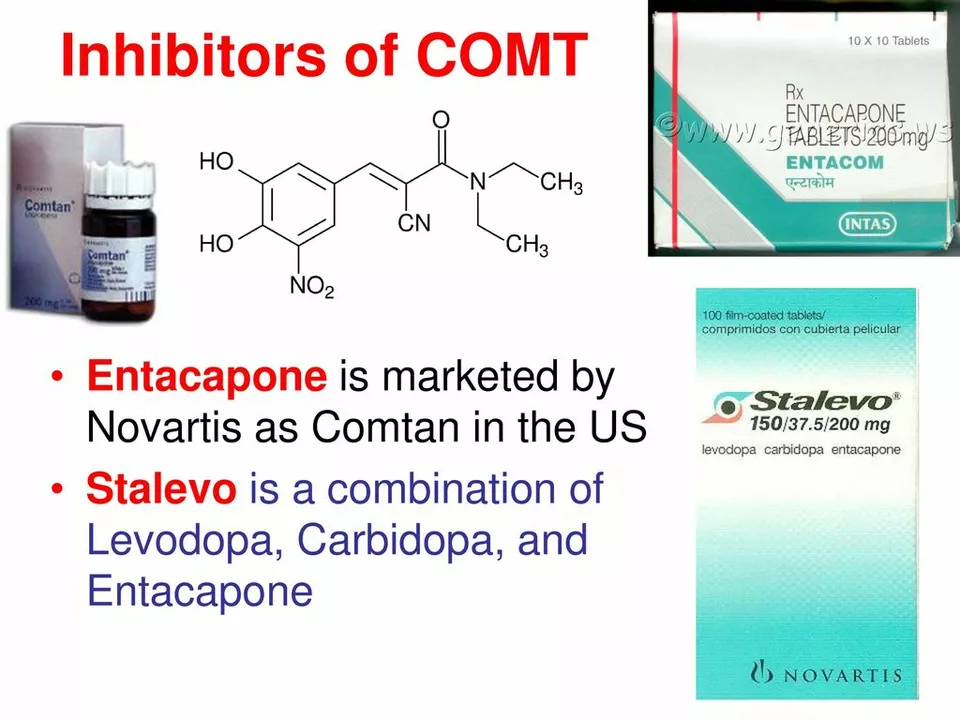
Medications are the foundation. Levodopa combined with carbidopa remains the most effective medicine to reduce slowness, stiffness, and tremor. Dopamine agonists like ropinirole and pramipexole can help too, especially early on or when levodopa causes side effects. MAO-B inhibitors such as selegiline or rasagiline slow symptom progression modestly and have fewer motor side effects. Amantadine can lower tremor and reduce dyskinesia for some people. Each drug has trade-offs — talk with a neurologist about timing, dose, and side effects you can expect.
Surgical options matter for the people who need them. Deep brain stimulation, or DBS, uses implanted electrodes to improve movement for patients whose medications no longer work well or cause severe dyskinesia. DBS is not a cure, but it can lower medication needs and improve quality of life. A thorough evaluation by a movement disorder team helps decide if surgery makes sense.
Therapy and daily life
Daily routines and therapy deliver gains. Physical therapy focuses on balance, walking, and strength. Speech therapy helps with voice volume and swallowing. Occupational therapy targets daily tasks so you stay independent longer. Simple habits—regular walking, balance exercises, and a consistent sleep schedule—show real benefits when done.
Medication safety and access are practical issues many face. If you order meds online, use licensed pharmacies, check for a valid prescription requirement, and read customer reviews. Avoid pharmacies that offer powerful drugs without a prescription. Keep an updated list of your medications, share it with every provider, and report new side effects quickly.
Managing non-movement symptoms makes a big difference. Depression, anxiety, constipation, and sleep problems are common and treatable. Talk to your doctor about antidepressants that work safely with Parkinson's medicines, or ask about behavioral therapies. Simple steps like fiber for constipation, light exposure for sleep, and gentle activity for mood help right away.
Planning ahead reduces stress. Set up medication reminders, label pill boxes, and discuss advance care preferences with family. Regular checkups with a neurologist help adjust treatment as the disease changes. Join a local support group or an online forum to swap tips and stay motivated.
If you want specifics—how ropinirole compares to other drugs, where to find reputable online pharmacies, or what to expect from DBS—check the detailed articles linked on this tag page. Use practical questions when you meet your care team: What benefit should I expect? What side effects should I watch for? When do we consider surgery?
Look for clinical trials if standard treatments stop working; many centers list trials and they often cover costs for visits. Caregivers should learn safe transfer techniques, set simple routines, and know emergency contacts. Small changes at home can make daily tasks easier and improve mood. Always ask questions early.