Endometrial cancer: what to know right now
Endometrial cancer starts in the lining of the uterus (the endometrium). It’s one of the most common gynecologic cancers, especially in people after menopause. The good news: it often causes symptoms early, so it’s usually found sooner than many other cancers.
Signs to watch for
The most important symptom is abnormal vaginal bleeding. If you’re past menopause and have any bleeding, see a doctor. If you’re still having periods, watch for heavier-than-usual flow or bleeding between periods. Other signs include pelvic pain, unusual vaginal discharge, and unexpected weight loss. Don’t ignore changes — early checks make a big difference.
Who’s at higher risk
Some factors raise the chances of endometrial cancer: being overweight, long-term exposure to extra estrogen (without progesterone), polycystic ovary syndrome (PCOS), diabetes, high blood pressure, taking tamoxifen for breast cancer, and older age. Having more pregnancies and using combined birth control pills lower the risk. Genetics matter too: a family history of Lynch syndrome increases risk and usually means earlier screening.
Diagnosis and what to expect
Your doctor will start with a pelvic exam. The next step is often a transvaginal ultrasound to check the thickness of the uterine lining. A tissue sample (endometrial biopsy) gives a clear answer — it’s quick and can be done in the clinic. If needed, a hysteroscopy lets the doctor look inside the uterus and take targeted samples. If cancer is found, CT, MRI, or ultrasound help stage the disease and plan treatment.
Treatment options explained simply
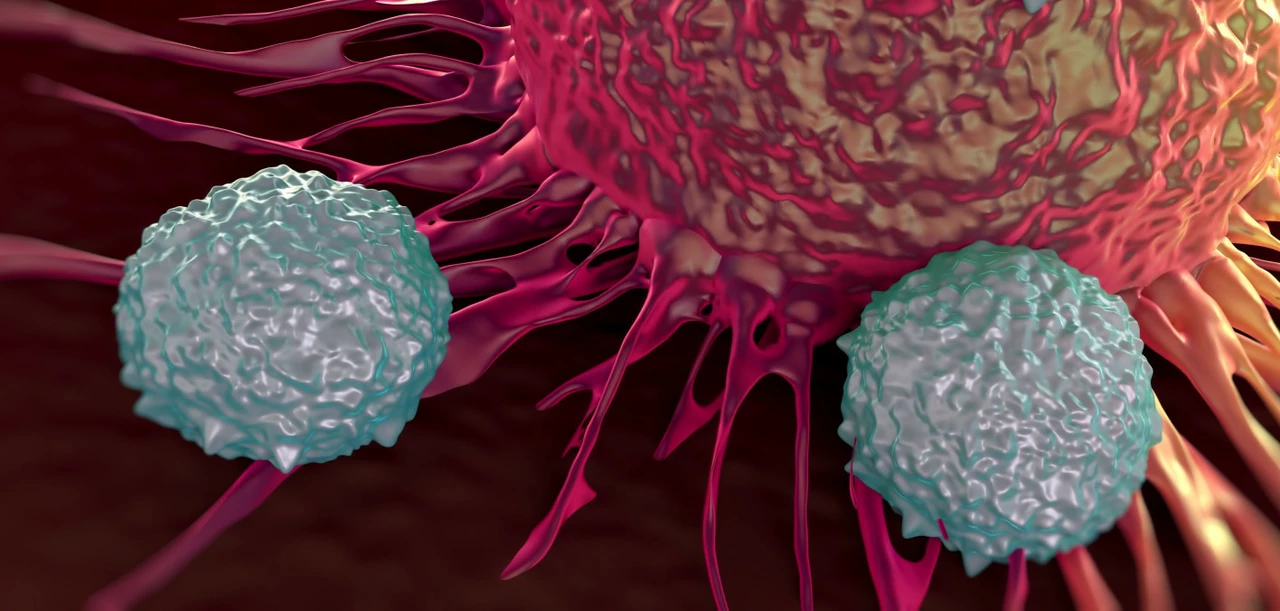
Surgery is the main treatment for most early cases. That usually means removing the uterus and often the fallopian tubes and ovaries. Lymph nodes may be checked during surgery. If the cancer is higher risk or spread, doctors may add radiation, chemotherapy, or hormone therapy (like progestins). For specific genetic profiles — for example, mismatch repair deficiency (dMMR) or MSI-high tumors — immunotherapy drugs such as pembrolizumab may be an option. Your care team will tailor treatment to the cancer stage, pathology, health, and personal goals.
After treatment, follow-up visits are important. These visits focus on recovery, watching for recurrence, and managing side effects like fatigue or menopausal symptoms after surgery.
Want to lower your risk? Keep a healthy weight, control blood sugar and blood pressure, stay active, and talk to your doctor about hormone therapy choices if you need them. If you have a strong family history of colorectal or endometrial cancer, ask about genetic testing for Lynch syndrome.
If you notice any abnormal bleeding or pelvic symptoms, don’t wait. Early evaluation gives you the best chance for simple, effective treatment and a faster recovery.